PD Catheter Placement - What to Expect
PD is quick to learn, easy to do, and puts you in charge. Getting a catheter placed can be the most alarming thing about it. Knowing what to expect—and what to ask—can help make it easier on you.
Know your catheter
PD catheters are soft and flexible. They are made of polyurethane or silicone, with one or two Dacron cuffs. One cuff is placed into the muscle wall of your belly. A second cuff may be placed in the skin at your exit site (where the catheter comes out of your body).

Exit Site
Your own fibrous tissue will grow into the cuff(s) and help anchor the catheter in place. The cuffs also help keep germs from going up the catheter.
The tip of the catheter in your body may be straight. Or, it may be coiled. Some have flat silicone discs to help hold your tissue layers apart so you can drain out the PD fluid better. Many designs have been tried, and they all have about the same results.1 Your surgeon may show you a picture of the type you will have. A PD catheter can be placed in the belly or in the chest (presternal).
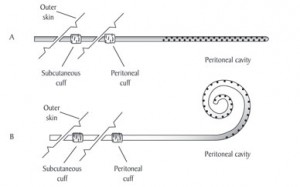
Diagram of a Catheter
Abdominal PD catheters
Placement in the belly is most common. The exit site tends to be an inch or so under the belly button. The catheter can be below your belly button or to the right or left of it. Tell your doctor where your belt falls so the catheter can go where it won't rub. The catheter must be kept clean and dry to avoid infection. You can take a shower with a PD catheter in your belly—but not a bath. Most programs do not suggest swimming. Swimming in a private pool or the ocean may be approved.
Abdominal Placement
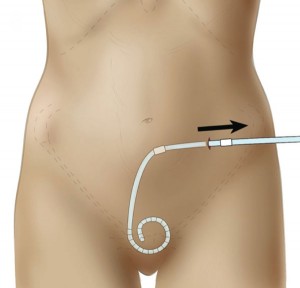
Abdominal Catheter
Catheter placement takes 15-30 minutes. It should be done in an operating room to help prevent infection. Nervous? Ask about drugs to help you relax or sleep. You won't be able to eat after midnight, so see if you can get a morning time. The nurse or doctor will draw on your skin with a marker to show where the catheter will go. Some centers will ask you to have an enema first. You may need to shower, too. Just before the procedure, you will need to empty your bladder if you make urine.
There are four ways to place an abdominal PD catheter:1
- Surgical
-
 This is the most common way to place a PD catheter. You will get local (just the area) or light general anesthesia. A scalpel is used to open the skin and muscle. Then, a tiny (1-2 cm) cut is made through the peritoneum (lining of the belly). Some
omentum
(a curtain of tissue inside the abdomen) may be taken out so it is not in the way. The catheter is pushed through the cut and then stitched around it. The exit site is chosen. A tunneling tool makes a place for the catheter under the skin. The catheter is pulled through the tunnel until the cuff is in place. Then stitches are placed around it. Surgery is costly and makes a larger scar than other techniques.
This is the most common way to place a PD catheter. You will get local (just the area) or light general anesthesia. A scalpel is used to open the skin and muscle. Then, a tiny (1-2 cm) cut is made through the peritoneum (lining of the belly). Some
omentum
(a curtain of tissue inside the abdomen) may be taken out so it is not in the way. The catheter is pushed through the cut and then stitched around it. The exit site is chosen. A tunneling tool makes a place for the catheter under the skin. The catheter is pulled through the tunnel until the cuff is in place. Then stitches are placed around it. Surgery is costly and makes a larger scar than other techniques.
- Trocar
- Using local anesthesia, a small (2-3 cm) cut is made through the skin and muscle. PD fluid will be placed in your belly with a needle or tube. Then, the surgeon will ask you to tense your stomach muscles while a trocar (pointed tool) is put in. The trocar is pulled out. Guides are left in to help the surgeon place the catheter and stitch it in place. Then a tunnel is made under the skin to an exit site, and stitches are placed around it. The trocar makes a large hole, so this technique may cause more leaks.1
- Guide Wire
- A small (1-2 cm) cut is made through the skin and muscle, with local anesthesia. You will be asked to tense your stomach muscles so the surgeon can push a small tube through the peritoneum. PD fluid will be placed in your belly. The surgeon will push a guide wire through the tube, and use it to place the catheter in the right spot. Then a tunnel is made under the skin to an exit site, and stitches are placed around it. This technique may cause less leaking. But, there is a risk of putting the small tube through the wall of the bowel.1
- Scope
-
Using local anesthesia, a small cut is made through the skin and muscle. A mini-trocar with a thin tube inside is inserted through the wall of the belly. The trocar is removed, and a scope is placed so the surgeon can see the inside of your belly. The catheter is placed and stitched. Then, the guide is removed. A tunnel is made under the skin to an exit site, and stitches are placed around it. A surgeon needs special training to use the scope.

Scope & Mini Trocar
Some surgeons keep the catheter under the skin for two weeks or more, instead of making an exit site. When it is time to start PD, a small cut is made to pull the catheter out. This is the Moncrief-Popovich procedure. Studies find that this technique helps catheters last longer. It also helps prevent infection.2
Presternal catheter

Presternal catheter
A presternal catheter is placed in the chest wall. The tip reaches down into the belly. The chest skin is thinner and less germy than the belly, so infection is less likely. Chest skin also moves less than belly skin, so this catheter is a good choice for a child or a heavy person. You can take tub baths with a presternal catheter, if you keep it out of the water. Swimming is not wise.
Before your catheter is placed, you can say if you want it to exit on the right or left side. Ladies: avoid your bra area, so the catheter won't rub. You will get IV antibiotics within 24 hours before the procedure. Using anesthesia, small (3-4 cm) cuts are made at the second and third rib and on the belly. Two parts of the catheter are placed. They are held in place with a titanium connector. Pockets are made under the skin to hold the cuffs.
Ask for a transfer set

Transfer Set
A "transfer set" is a 4-6 inch length of tubing with a titanium valve. The transfer set lets the catheter open and close. Ask the surgeon to put one on in the operating room-it takes seconds. If this isn't done, it may take 30-45 minutes to put one on in the clinic, and the risk of infection is higher.
When you do PD, your transfer sets will need to be changed every 6 months. This is a sterile procedure. It can be done in the clinic, or you can learn to do it at home yourself.
How you may feel afterward
Most people say that they don't feel much pain after having a PD catheter placed. Some are hungry because they had to fast for a few hours. Some get right up and don't need pain killers. Others do have some pain for 3-5 days, take pain pills, and find it hard to wear pants.
If you had general anesthesia, you may feel groggy. You may also have some nausea. Since you don't know how you will feel, plan to take it easy for a few days so you can heal.
Caring for your new catheter
PD fluid may be put in your belly when a catheter is placed. If so, some may drain out and soak the bandages. You should get clean, dry gauze and tape to take home just in case. Your belly may also feel tight if fluid was left in. This will ease up over time.

In most cases, your PD training nurse will want to change your dressings. This gives him or her a chance to check on your healing. Once your site looks good, you may be asked to leave off the dressings so it can heal in the open air.
At a clinic visit, your PD nurse will flush your catheter with fluid to see how well it drains. To do this, he or she will add a tubing extension onto your transfer set:
- Ask if you have a choice about length. It is easier to care for a shorter catheter.
- A bag of fluid will hang from an IV pole and drain into your belly through the catheter. Unless the fluid is cold, you may not feel this.
- If the flush goes well, you'll be ready for training.
Often, training can start a week or two after getting your catheter.
What can go wrong?
No treatment is perfect. Any type of access has its challenges. So, when you read this section, keep in mind that most of these issues can be prevented with good, careful technique.

One key to PD success is keeping germs out of your catheter and your belly. It's not easy. Germs are all over. But you'll learn steps for aseptic (germ-free) technique that you'll need to follow closely. It will seem like a lot to learn at first. But, the steps will quickly become a habit—like brushing your teeth-that you can do without thinking too much about it.
Some types of infection that can occur with a PD catheter include:
- Exit site infection
- Germs grow in the skin around your exit site. Some clinics will have you use an antibiotic cream for exit site care. Mupirocin can reduce infection by about 2/3.3 %sup 3 Others will have you air dry your exit site so it is not moist. (Germs love moisture.) If you get an exit site infection, your doctor will prescribe antibiotics. An exit site infection can lead to a tunnel infection.
- Tunnel infection
- Germs grow in the tunnel under your skin where the catheter goes. This infection can be hard to get rid of. And, it can reach your peritoneum. Your doctor will prescribe antibiotics. You may need to get a new catheter if the infection does not clear.
- Peritonitis
- Germs grow in the peritoneum. This can be painful and can cause scarring. In some cases, scarring can make it impossible to keep doing PD. You'll learn to watch for cloudy fluid and report pain right away so you can start antibiotics.
Other problems that are not infections can also occur with a PD catheter:
- Migration
- Sometimes a PD catheter won't stay down in the belly. It may drift up under your ribs, where it can cause pain. An X-ray will show this. The catheter may move back down by itself. This is often the case if you were constipated and take a laxative. Rarely, surgery is needed to move the catheter back where it belongs.
- Problems draining
-
In rare cases, the catheter can be blocked by:
- Blood clots
- Fibrin (a blood protein)
- Omentum tissue
- Hernia
- A weak spot in the muscle of the belly or groin. The extra pressure of fluid in the belly can cause or reveal a hernia. In men, this can show up as PD fluid that leaks into the scrotum (inguinal hernia). A minor surgery with mesh to make the muscle stronger can fix this problem.
- Body image concerns
- Looking down and seeing a tube coming out of your body takes some getting used to. How you feel about yourself and your body can affect your sex life and your relationships.

If you have a partner, talk about your feelings. You may find that your loved one is so happy to have you around and able to do PD that the tube bothers you more than it does him or her. If you don't have a partner, don't assume that the PD tube means that no one will want you! We all have our scars. No one is perfect. And you are so much more than your body.
Some people cover the tube with gauze so they don't have to look at it much. That's okay. Most people on PD do find that they get used to the catheter in time. Visit the Sexuality and Fertility module of Kidney School™ to learn more about how to cope with a PD catheter.
Conclusion
Getting a PD catheter placed is a first step toward a treatment that is flexible, convenient, and easy to learn and do. If you take good care of your PD catheter, it will help you feel your best.
References:
- Ash SR, Daugirdas JT. Peritoneal Access Devices. In Handbook of Dialysis, Third Edition, John T. Daugirdas, Peter G. Blake, Todd. S. Ing. Lippincott Williams & Wilkins, Philadelphia, 2001.
- Dasgupta MK. Moncrief-Popovich catheter and implantation technique: the AV fistula of peritoneal dialysis. Adv Ren Replace Ther. 2002 Apr;9(2):116-24.
- Tacconelli E, Carmeli Y, Aizer A, Ferreira G, Foreman MG, D'Agata EM. Mupirocin prophylaxis to prevent Staphylococcus aureus infection in patients undergoing dialysis: a meta-analysis. Clin Infect Dis. 2003 Dec15;37(12):1629-38.

