Self Cannulation: A Sticking Point

With a background in Biology and endless bloody dissections I came to HD with little aversion to needles and began self-cannulating during my first week of training. My clinic teaches solely the ladder technique in the belief that the 4% increased infection potential with buttonholing is not worth the risk.
In spite of great care I had several infiltrations in those early days with attendant bruising causing widespread discoloration of my arm (below), persisting after many months.
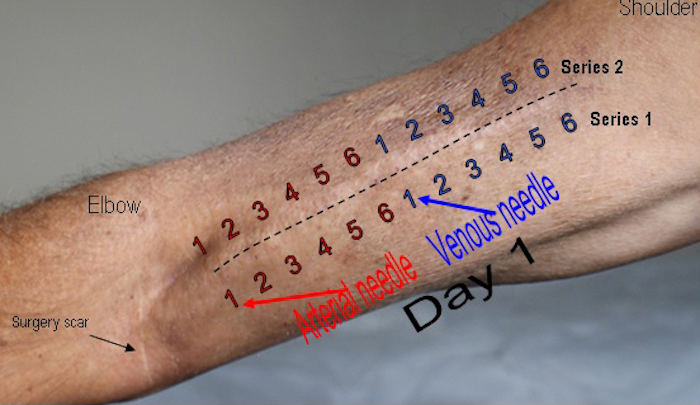
Those of us who use ladder needling have been advised to spread the sticks as widely as possible over the length of the fistula to avoid what has been unimaginatively termed "one-site-itis,"- the outcome of the weakening of the vessel wall due to repeated penetrations in one spot. Places of damage often lead to aneurisms. Proper needle site rotation is essential to ensure even development of fibrous tissue along the fistula’s length so that there are no weak spots. Early in training my renal nurse advised the vessel should be cannulated from the sides (Series 1 and 2 in the image) as well as on top along the median to greatly expand the number of sticking sites.
How to space the needling? A scan of the literature suggests 6.3 mm minimum between successive entry points and 70 mm between arterial needle entry and venous needle entry on any given session. To maximise the entire fistula length, especially in the case of my shorter upper arm one, I plotted a "sticking map" to convince myself I had plenty of room to avoid the dreaded "one-site-itis."
A stick is done at each number: lower red "arterial 1" is matched with lower blue "venous 1". Then on to the "twos" By the time blue venous 6 is reached red arterial 6 is closing in on blue venous 1’s earlier entry point and its time to move over to the other side of the fistula (Series 2) where the sequence is repeated.
The dashed line shows the fistula median and marks further access for six sessions in the same manner. So in all that’s 18 tx sessions (@ 4 sessions per week), or at least 4 weeks before a needle re-enters a previously cannulated site.


Comments
Jeff Stumpe
Feb 15, 2017 5:56 PM
While learned buttonholing during HHD training, it was not long before I felt the need to develop a third buttonhole site to accompany the two that were developed for me during HHD training.
Tentative at first, I did develop the requisite skill set to competently cannulate with 15 GA sharp dialysis needles. The wisdom to then create and use additional buttonhole sites has allowed me to abandon sites when they can no longer be cannulated with 15 GA blunts owed to changes in the fistula flap access.
Over the past 4-1/2 years, I have had to abandon 7 different sites including the two that were developed during training.
I've settled on five buttonhole sites on my three vessel fistula that features two separate venous returns, giving me 9 different working Arterial/Venous combinations with only one of these combinations occurring on the same vessel and balance between vessels.
It is a very unique fistula that started as a single vessel from anastomosis in my right wrist and expanded to the three vessels on my forearm after a fistulagram and stenosis removal just two weeks after starting HHD training.
I have maximized the utilization thereof, and in spite of clotting off (and subsequent declotting and fistulagram) each venous return at least once since May 2014, I've not missed a single treatment or needed a CVC because I had a second venous return available for my HHD treatments.
Keeping all 5 buttonholes active is a challenge owed to the natural healing process and an alternating 5, 4, 5 weekly treatment schedule.
I am very aggressive in scab removal and buttonhole site prep - the chief sources for buttonhole technique infections.
My reward for buttonhole cannulation is the absence of painful and treatment stopping infiltrations and never missing an HHD treatment in 4-1/2 years.
Ant
Feb 17, 2017 6:32 AM
DebraNull
Jan 27, 2017 11:30 PM
Talker
Jan 27, 2017 2:55 PM
Thanks
Lisa Goodwin
Jan 27, 2017 1:21 PM
Ant
Jan 28, 2017 9:40 PM
Meantime I've improved the rather tatty image and saved the document as a PDF. I can forward this to you if you'd like but will need an email contact.
Sheree B
Jan 27, 2017 1:21 AM
Richard Vallone
Jan 26, 2017 11:24 PM
Richard Vallone
Ant
Jan 27, 2017 2:05 AM
Sorry to hear of your needle and pressure difficulties.
Sounds like the tip of the needle is either lying too superficially or is pressing against one of the vessel walls. Here's what works for me:
Once I've decided the exact entry point for the needle I make a spot there with a felt and then draw a thin line to mark the exact direction the needle will follow once under the skin. Tourniquet is optional (I don't). Next I rest the needle tip lightly on the spot then check the needle shaft is true-aligned to exactly follow the path I've drawn. I check on this again once the needle is 3 mm in and the blood flashback looks good, before sliding it the rest of the way in.
Bad pressure can sometimes be overcome by placing a small wad of gauze under the needle hilt against the skin (needle tip pressing on vessel upper wall) or by withdrawing the needle a few mm (needle tip against a side wall or lower wall)