Local Anesthetic for Hemodialysis Needles in Short Supply: Where’s the EMLA?

“This morning a dialysis tech asked if I needed more binders. I don't. But I told her I was almost out of and needed more numbing cream. Cream had usually been ordered through dialysis and I received by mail. Tech told me the company that made it went bankrupt and the cream would no longer be available. That we now will have to come to dialysis early and they will have patches they will apply. She has never seen or used them and doesn't know how big they are or how long it will take for them to become effective. We have received no notice from the clinic or the pharmacy who sends the cream. I find this very frustrating that the cream will no longer be available and we were not given notice. If I hadn't asked about making sure my cream had been ordered I guess I would not have been told until it was too late. Has anyone else heard this or used the patches before? I put on the cream at least an hour before dialysis. So now will I have to come into dialysis an hour earlier? I asked another tech and the head nurse but they said they did not know either. I asked the nurse to find out and he just came back and told me one minute. Sounds odd to me but maybe it works like the numbing spray they have used at the hospital? Anyone have any further info about the patches?”
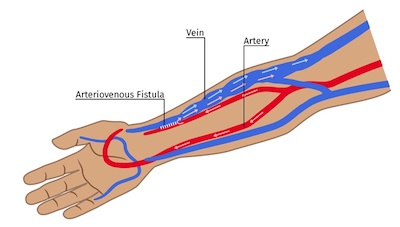
We’ve been picking up signals like the one above on social media for several months that there are nationwide shortages of EMLA—the prescription-only (in the U.S.—it is over-the-counter in the UK) eutectic mixture of local anesthetics (2.5% lidocaine and 2.5% prilocaine) many dialysis clinics offer patients to numb insertion of the 14 or 15 gauge steel needles used in the U.S. for hemodialysis. (Fun fact: Eutectic means the melting point of the two drugs together is lower than that of the individual drugs. EMLA’s melting point is below room temperature.)
Current EMLA Availability
AstraZeneca’s 1985 patent (U.S. Pat. No. 4,562,060A) for EMLA expired in 2005, clearing the way for generic versions of the drug. AstraZeneca no longer makes EMLA and Akorn, one of the manufacturers, has shut down. Other companies continue to manufacture and/or sell EMLA:
How Well Does EMLA Work?
EMLA’s package insert states that the product should be applied under an occlusive dressing for at least one hour (my emphasis). “Satisfactory dermal analgesia is achieved 1 hour after application, reaches maximum at 2-3 hours, and persists for 1-2 hours after removal.” For patients with deep fistulas, 1 hour may not be long enough. A blob of cream 1/8” thick and the size of a dime over each needle site is enough. NOTE: An occlusive dressing—such as Tegaderm®, kitchen plastic wrap, Press N’Seal wrap, or Saniderm tattoo dressings—keep the product on the skin and off clothes, and hold in warmth so the EMLA will more effectively soak into the skin. Washing skin oils off prior to application is also wise.
According to WebMD, EMLA patches do not work any faster than the cream. At least an hour is needed. Why won’t dialysis clinics give patients patches to apply at home before treatment? I don’t know, and it makes zero sense to me. Perhaps someone could explain the rationale in the comments?
Does EMLA’s combination work better than other lidocaine creams for needle cannulation? Perhaps, suggest studies. In a small RCT, 29 healthy adults tested the numbing capability to blunt or sharp stimuli of eight compositions of creams left on for 20, 40, or 60 minutes.1 After 60 minutes, 20% lidocaine cream alone was more effective than placebo—and equally effective as lidocaine with prilocaine. A cream with 10% lidocaine and trometamol was significantly better than placebo—and not worse than lidocaine with prilocaine. It worked faster, too. Yet, another small study (n=24) received EMLA cream on the dorsum of one hand, and lidocaine tape on the other hand.2 One group received IV cannulation on the EMLA hand first and then the tape hand; the other group on the tape hand first and then the EMLA hand. Cannulation was significantly less painful when the EMLA cream was used. A meta-analysis of 20 papers that excluded comparative studies did find EMLA to have “a large significant effect,” on venipuncture and IV insertion pain regardless of age, type of pain scale, insertion site, premedication, funding, or study design, in 85% of the tested population.3

An FDA-approved EMLA Alternative
Can’t get EMLA? Can’t use it due to an allergy to a component ingredient? An array of 4% or 5% lidocaine-only, over-the-counter pain creams such as LMX-4 are available at drugstores or online. Some are advertised for helping to prevent tattoo pain.
Drug-free ways to address needle fear and pain are also an option. Ice alone, or distraction can help. So can pulling the skin taut.
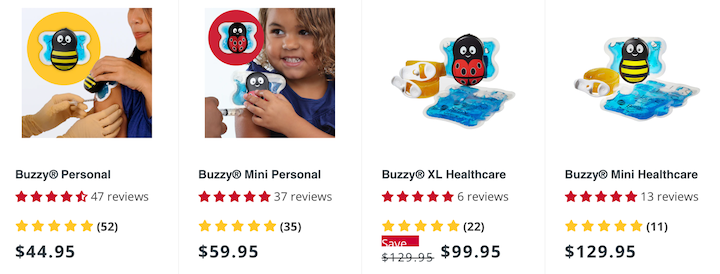
Pain Care Labs, which has been making, “game-changing wearable pain relief” since 2009 recently received FDA 510K clearance for the Buzzy Pro, a $149 device for dialysis clinics that combines high-frequency vibration with optional ice to numb venipuncture for blood draws or dialysis cannulation. Or, for home use, the original Buzzy, developed for pediatrics, comes in different sizes, and works in the same way. The Buzzy devices are supported by more than 75 peer reviewed studies, and you can download a 2023 White Paper entitled Addressing Needle Dread, Fear, and Phobia 2023 from the website.
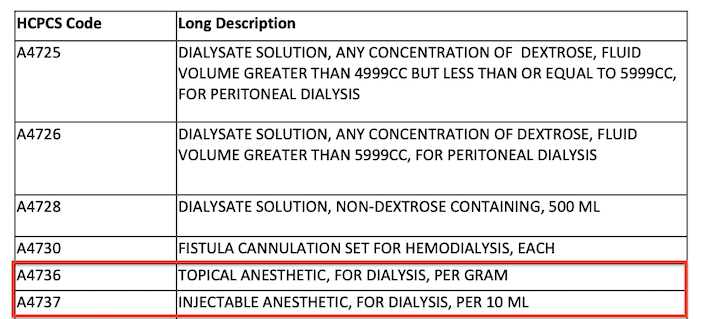
Patients who are subject to repeated cannulation with large-bore needles deserve to have their fear and pain addressed. Clinic staff may not be aware that Medicare requires clinics to provide topical and injectable anesthetics to patients at no charge, as part of the Bundle of care. To ensure that patients receive the relief they need, clinics can find alternative sourcing of EMLA or use other products.
Weilbach C, Hoppe C, Karst M, Winterhalter M, Raymondos K, Schultz A, Rahe-Meyer N. Effectiveness of various formulations of local anesthetics and additives for topical anesthesia – a prospective, randomized, double-blind, placebo-controlled study. J Pain Res. 2017;10:1105-1109↩︎
Matsumoto T, Chaki T, Hirata N, Yamakage M. The eutectic mixture local anesthetic (EMLA) cream is more effective on venipuncture pain compared with lidocaine tape in the same patients. JA Clin Rep. 2018;4:73↩︎
Fetzer SJ. Reducting venipuncture and intravenous insertion pain with eutectic mixture of local anesthetic: a meta-analysis. Nurs Res. 2002 Mar/Apr;51(2):119-124↩︎


Comments