From Nephrology to “Healthcare”: Reflections on Attending the IHI Meeting

I’ve traveled a lot this fall, and noticed that just about every time I get off of an airplane, there are at least five wheelchairs waiting. What does that have to do with the experience of attending my first annual meeting of the Institute for Healthcare Improvement (IHI)? Quite a bit, as it turns out.
The IHI is the darling of CMS, which has enthusiastically embraced (but changed the name of) the IHI’s “triple aim” for healthcare improvement :[1]
- Improving the patient experience of care (including quality and satisfaction)
- Improving the health of populations
- Reducing the per capita cost of healthcare
In fact, Don Berwick, MD, the former President and CEO of IHI received a recess appointment from President Obama to lead CMS and the Center for Medicare and Medicaid Improvement—a shining time at CMS (IMHO) that ended when he resigned due to partisan bickering. (Who would want a visionary expert in healthcare improvement to run CMS? Apparently only half of Congress…)
As the IHI rightly points out, the US has the most costly healthcare in the world (using 17% of our GDP). And, we have some of the worst big picture outcomes in the first world :
- We are, according to the CIA (yes, that CIA), ranked 56th in the world for infant mortality, considerably worse than the Czech republic, Belarus, South Korea, and Slovenia.[2]
- We are ranked 42nd in the world for life expectancy at birth.[3]
- We rank dead last for overall healthcare, vs. Australia, Canada, most of Europe, Sweden, and Norway.[4]
When Chris Sarfaty, a renal social worker and passionate IHI attendee invited me to become part of a panel she was planning to propose to IHI with Richard Gibney, a nephrologist who has transformed his practice entirely, based on his IHI learnings; Britt-Mari Banck, a nurse from Sweden who has set up a fabulous in-center self-care clinic; and Nancy Spaeth—one of the longest-surviving ESRD patients in the U.S., I was honored. And, if I do say so myself, we put on a terrific workshop!
And, then, there we were at the meeting. Well, kind of . IHI supports itself in part through this meeting—which costs $1,200. So, the 5,500 or so attendees represented about $6.6 million in revenue, but they did not comp the travel or meeting registration for all speakers. Our group of five got two registrations, and Nancy got a third as a “Patient and Family Advisor.” So, MEI got a booth, and I went to the keynote talks and faculty reception (which was wonderful).
There were a lot of bright spots. So many passionate, curious people who wanted to improve healthcare! So much focus on improving the patient experience! Fabulous “blue shirt” staff who answered questions, guided us to sessions, and went out of their way to make sure that everyone’s needs were met! Listening to keynotes from Maureen Bisognano, the IHI CEO, Atul Gawande (!!!), Robin Roberts (from Good Morning America), and Don Berwick himself was a huge plus. And, meeting Maureen and Don at the faculty reception was the biggest thrill of all. I got to show them both our dialysis decision aid, My Life, My Dialysis Choice, which asks the key question of the meeting for patient engagement: “What Matters to You?”
But, I live and breathe chronic disease. Half of us Americans have at least one (which generates 84% of U.S. healthcare spending), and 7 of our top 10 causes of death are chronic.[5] One third of us are obese. Half of us don’t exercise. Chronic disease is an enormous healthcare problem—but, as far as I can tell, it is largely ignored by IHI, despite the “health of populations” part of the triple aim . There was just one session on CKD at the meeting, plus our preconference workshop, which had 7 attendees. In the exhibit hall, we had the only booth that focused on a chronic disease.
In Maureen’s talk, about adding the “and” to healthcare (“Quality and cost” “Health and Healthcare”), I have to admit that I cringed a little when one of her examples was improving the flow for joint replacement surgeries, which are, apparently, a huge growth area in U.S. medicine. Why not address the root cause—obesity and a highly processed, chemical-laden, genetically modified food supply—so we can live out our lives with our original joints? Chronic disease and obesity may be why five people getting off of every airplane need wheelchairs!
CKD, in particular, is one of the most costly conditions CMS covers. Ten percent of the Medicare population has CKD—which accounts for nearly 20% of total Medicare costs.[6] End-stage renal disease (ESRD) costs rose to $28.6 billion in 2012—or 5.6% of the Medicare spend. So, CKD plus ESRD use a staggering 24% of the total Medicare budget.
And, do we get good CKD outcomes as a result? Well…no. No, we don’t.
- Each year more than 35% of people with CKD (I’ve heard as many as 50%) “crash” into ESRD and need emergent dialysis, showing a distinct lack of coordination of care, ineffective education that did not help people overcome their fear and denial—or both .[7]
- Survival on dialysis in Japan is triple what it is here, and we are also trounced by Australia/New Zealand, Italy, France, the UK, and Germany. [8]
- According to the most recent United States Renal Data System report, 89% of people on dialysis in the U.S. use standard in-center hemodialysis—which has the poorest outcomes at the highest cost—and is an option that just 6% of U.S. nephrologists would choose for themselves if their own kidneys failed .[9]
- It’s not surprising that nephrologists would not choose a treatment that would give them two days in a row with no blood cleaning. It was first observed in 1999 that the thrice weekly pattern of hemodialysis causes 50% more sudden deaths on the day after the “killer gap”. [10] In fact, in the 12 hours before that next Monday or Tuesday treatment after the weekend, the risk of death is triple.[11] “Standard in-center” HD is clearly NOT a physiologic treatment!
- Home dialysis—peritoneal dialysis, daily home HD, “extended” HD done at night during sleep offers better outcomes and longer survival than standard in-center HD .
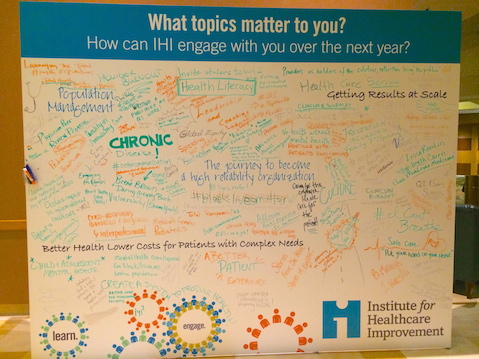
So, overall? My impression from this meeting is that right now, “IHI” more appropriately stands for Institute for Hospital Improvement—not healthcare improvement. Since any of us could be in the hospital at any time, it’s certainly important to ensure that hospitals are safe places to receive high-quality care. But, it would be amazing to see the IHI devote some of the same passion and resources that hospitals now enjoy to primary prevention of chronic disease . In fact, I wrote this on their idea board. I hope they’ll think about it.
[7] Owen WF Jr. Patterns of care for patients with chronic kidney disease in the United States: Dying for improvement. J Am Soc Nephrol. 2003. 14:S76-80
[8] Robinson BM, Zhang J, Morgenstern H, Bradbury BD, Ng LJ, McCullough KP, Gillespie BW, Hakim R, Rayner H, Fort J, Akizawa T, Tentori F, Pisoni RL. Worldwide, mortality risk is high soon after initiation of dialysis. Kidney Int. 2013 85,158-65
[9] Merighi JR, Schatell DR, Bragg-Gresham JL, Witten B, Mehrotra R. Insights into nephrologist training, clinical practice, and dialysis choice. Hemodial Int. 2012 Apr;16(2):242-51
[10] Bleyer AJ, Russell GB, Satko SG. Sudden and cardiac death rates in hemodialysis patients. Kidney Int. 1999. 55:1553-9
[11] Bleyer AJ, Hartman J, Brannon PC, Reeves-Daniel A, Satko SG, Russell G. Characteristics of sudden death in hemodialysis patients. Kidney Int. 2006 Jun;69(12):2268-73



Comments
nieltje
Dec 12, 2014 10:43 PM