Why I Think “I prefer to Dialyse in Unit – in Case Anything Goes Wrong” is a Fallacy that Needs Addressing

I’ve been on dialysis for 6 years now; the first year on peritoneal dialysis (PD), then 8 months in my local hospital (in the UK) doing hemodialysis (HD) and the rest on home hemodialysis (HHD). I’ve gotten increasingly involved in patient groups on Facebook and with my local hospital and other NHS trusts. My specific goal is trying to improve dialysis pathways for patients and encourage more patients to get a) engaged with their care and b) to try home dialysis, as I believe the standard 12 hours, 3 times a week 4 hours at a time, isn’t the optimal way to deliver dialysis as a renal replacement therapy. It’s not my intention to discuss the merits of in-unit HD and PD, as this post is really about HHD.

I’ve reached that conclusion based on a little internet ‘research’ – initially from the Kidneyviews blogs of Professor John Agar and others on Home Dialysis Central. Then came the webinars in the Wisdom from Dr Agar series, as well as discussions with other experienced, long-term HHD patients whose opinions and experiences I’ve grown to value and respect and from my own ever-growing experience and from discussions with my Nephrologists and nursing team.
Timing is Everything
The decision of where to get your dialysis either home via PD or HHD or in a hospital or clinic setting is one that confronts patients at a truly terrible time: heath is declining, energy levels are low, thought processes are dulled by an increased toxic load—all on top of the emotional strain with fears of mortality at worst and an uncertain future at best. And, the financial implications–bad enough here in the UK, but a considerably bigger issue in other countries that don’t have the benefit of universal healthcare or a welfare system I’ve discovered.
I’ve seen that new patients reach out on patient groups on Facebook (my social media of choice because I’m in my 50’s) and I often see posts that pose the frequently linked issues/questions “What’s your preference: Home or In centre?” and/or “Home or In centre - Pros and Cons” and what follows are amongst the most commented threads of that week as people, I’m assuming well meaning, splurge forth their opinions—and herein lies one of the problems as I see it. Most people aren’t actually expressing an opinion of their preference, because they’ve not experienced dialysis in both settings to be able to give a “value” judgement comparing one with the other.
It seems to me that what they’re actually doing is expressing their opinions on why they made their choices, and as the numbers doing dialysis in-centre are so much greater (just 51 UK new patients started on HHD, while 1715 started on PD and 5838 started in centre in 2021) the home dialysis message needs to fight to prevent itself being swallowed and eventually drowned by the weight of numbers. One of the most common “reasons” for “preferring” in-centre seems to be a variation on,“I prefer in-centre as you’re taken care of if something goes wrong.” It seems to me that this is only ever suggested as a reason why in-centre is better than HHD by someone who appears to have no experience whatsoever of HHD.
Two Main Worries

So what exactly is the “something” that in-centre patients are worried about going wrong? I’ve probed this point—probably to the point of appearing rude to some people—and it seems to me that there are in fact TWO “somethings” that loom large as fears of things that might go wrong to in-centre patients, and the fact that they’re all together 12 hours a week “chatting it through” (when, in fact, what they’re doing is sitting in an echo chamber that’s repeating their fears back to them and reinforcing them) and it’s up to US—the HHD patients to shout loudly to level the playing field in these online patient groups with regard to these two issues:
1- The Hypo (Hypotension blackout)
In the short period I was in hospital getting HD, I had a hypo myself. I felt it coming, but had no idea what it was. One minute I was sat up in a chair on a quiet ward with two other patients and a nurse sat at the desk beside me doing the shift paperwork, and the next thing I knew, I was reclined beyond the horizontal with four or five nurses, and on the receiving end of saline resuscitation.
I had been significantly overloaded with fluid when I started HD in unit—over 20 litres (and therefore 20 kg) above my dry weight, and we’d been removing fluid (ultrafiltration—UF) at 1 litre per hour, the maximum permitted. So, we were removing four of those litres over the 4-hour session, and on that day it was just too much for me. It was scary and disorienting...and for anyone looking on, it must have been awful.
If patients in centre are seeing frequent hypos (and I fear they are)—it’s no wonder they look on in horror and ask themselves and repeat on social media, “How could you possibly deal with that – at home—on your own with no trained staff there to help you?”
The simple answer is –it won’t happen, because you’ll be trained in how to avoid it!
In the sessions after my hypo, I talked over what happened and WHY IT HAD HAPPENED with the staff and read some articles,1,2 and this quote from Dr Agar stood out to me:
“At a symptom level, short dialysis treatments are symptom-rich;
long treatments are symptom-free. Shorter treatments induce
ever more cramp, hypotension, and misery. “
This was the seed in my mind that made me find a better way of getting my treatment because I want the rest of my life to be happy, joyful, and long! I wanted to find a way of getting the “good dialysis.”
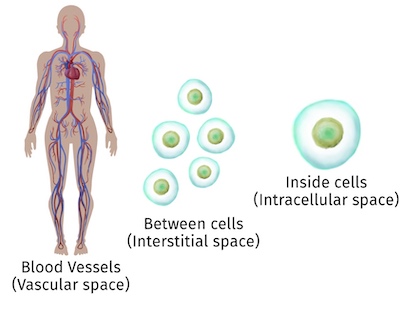
I learned about fluid movement within the body and the way to safely remove it at home without causing the symptoms of a hypo. We can only remove the fluid from the blood, and it takes time for fluid in the cells and between the cells to refill the blood. If we take too much fluid too quickly from the blood, blood pressure drops—inducing blackouts (and other issues). I’ve discovered that in fact MY BODY could tolerate a maximum UF rate of 600ml/hour before I got symptoms of volume collapse and “dialysis hangover” effects like exhaustion. So, for my personal safety and comfort I’ve agreed with my team on a buffer below that, and will take off no more than 400 ml/hour UF. Now, I do my dialysis overnight for at least 8 hours at a time and normally do dialysis every other night. This UF rate gives me the potential to remove a total of 3.2 litres over the 8 hours. If there are more than 3.2 litres to remove, there are two ways for me to remove it: stay on the machine longer (8.5 or 9 hours are choices I often make) or do an extra treatment.
As a result of the training and my learning and making sure the UF rate is well within the limits that my body can safely tolerate I’ve never even come close to repeating the hypo I suffered while I was in the hospital during any home hemo treatment. In fact, on a couple of occasions the UF rate has been low enough that my blood pressure has actually increased a little during treatment!
So, what of the other “something”?
2 – A needle coming out.
This is a big one, and I had had all those thoughts myself, BEFORE I DID MY TRAINING. I was always planning to be doing dialysis in an empty house alone while my wife was at work…but I’m going to let you into a secret now: my needles come out every time I do dialysis, and I’m sure yours will, too, because none of us are walking around with dialysis needles in our arms!
How to remove needles safely and stop the bleed is a vital part of the training. An unplanned needle removal differs only in the amount of preparation you’ve done for that moment, but the procedure is the same: stop the bleed!
When I switched to overnight treatment I was scared I’d lose a needle in my sleep, but proper needle taping technique can and should reduce the fear.3 During my training, I tried to deliberately pull the needle (safely still in its sheath not inserted in my vein) away from the taping and can’t do it—I’m not strong enough—so I’m now really confident that I’m not going to accidentally turn over in my sleep and dislodge a needle, and I sleep soundly.

Before I came home however, I was told by other patients and by staff of an unnamed patient who had been dialysing at home alone and had lost a needle and bled to death. It’s a horror story that seems to be told in units across the world, but the 2021 Renal Registry Report in its mortality chart for HHD patients reports ZERO deaths as a result of needle dislodgement in the period the report covers (2012- 2021). Likewise, a Google search for the same information produced no results for HHD patients—but sadly did reveal a small number of results for deaths by needle dislodgement in the UK in recent years that happened to patients IN UNIT!
I’d be extremely surprised if the results were much different elsewhere. In preparation for this post, I considered articles about mortality rates in AUS/NZ and USA that seem to reflect the same, although I’ve not referenced them, as I’m writing about my thoughts experiences and that’s all to do with the UK.
So it seems to me, that when we see “I prefer to dialyse in unit – in case anything goes wrong” in its various guises, we owe it to ourselves and to the patients facing that Hobson’s choice about dialysis and reaching out for guidance about how to make that decision we need to be strong and vocal and insist – those things going wrong that you’re worried about – they’re happening BECAUSE you’re in-unit!
References
Agar J. Don’t flog the fistulas. KidneyViews blog post. 3/14/2014 https://homedialysis.org/news-and-research/blog/535-dont-flog-fistulas-slow-hemodialysis-blood-flow
Agar J. Dialysis 101 for home hemodialysis. KidneyViews blog post. 4/19/2019. https://homedialysis.org/news-and-research/blog/304-dialysis-101-for-home-hemodialysis-hd
Chan DYF, Dobson S, Barber T. Hemodialysis taping styles and their effect on reducing the chance of venous needle dislodgement. Sem Dial. 2021 May/Jun;34(3):218-223


Comments
Nancy Verdin
Jun 27, 2023 4:29 PM
Chris Gillanders
Jun 25, 2023 6:56 PM
Chris Gillanders