Dialysis Is Life-Saving, but Not Perfect: We Can Do Better

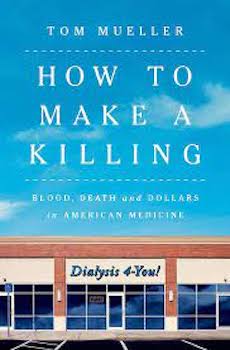
On August 1, Tom Mueller’s book How to Make a Killing: Blood, Death and dollars in American Medicine was published on the dialysis industry. It has created quite a stir among dialysis providers with some criticizing his reporting. Mueller collected data and interviewed patients, family members, patient advocates, nephrologists, current and former dialysis staff of all disciplines, attorneys, union leaders, healthcare policy experts, and economists. He even interviewed nephrologists and nurses from other countries. For his research, he also visited dialysis clinics. His book starts with the history of dialysis and the changes that have made it what it has become, a miracle procedure that saves lives—but at a high cost to the government, insurers, and patients.

Mueller spoke to several dialysis history-makers like Dr. Chris Blagg who led Northwest Kidney Centers for 27 years. Dr. Blagg saw many changes in dialysis from the early days when dialysis was done in hospitals and many patients were trained to do dialysis at home. Dr. Blagg wrote 149 peer-reviewed articles about dialysis and a book about the history of Northwest Kidney Centers.1 I served with Dr. Blagg on the Life Options Rehabilitation Advisory Council (LORAC), a program founded by the Medical Education Institute (MEI) in 1993 that included nephrologists and all disciplines of dialysis staff plus an exercise physiologist. Dr. Blagg and Life Options advocated with patients, staff and policymakers in support of home dialysis and rehabilitation. Dr. Blagg died in 2022.

Mueller interviewed multiple patients, including Nancy Spaeth, who lived the longest after kidney failure—56 years. Nancy was selected for dialysis by the life and death committee and started dialysis in 1966 as a patient of Dr. Belding Scribner, a dialysis pioneer who invented the Scribner shunt. Nancy started on in-center HD, but 2 years later was trained to do HD at home and did nocturnal HD. Over the course of kidney failure, Nancy had four transplants. After her kidneys failed, she attended college, married, raised two children, and worked as a teacher and nurse. Nancy also served with me on MEI’s LORAC. She gave multiple presentations across the U.S. and overseas and preached a salt limit, which helped her stay healthy. She advocated with healthcare professionals and policymakers for rehab, nutrition education and home dialysis. Nancy died in 2022.2
Mueller’s book addresses the history of Medicare coverage of dialysis and transplant and how the 1972 law that provided that coverage unwittingly hurt home dialysis by paying doctors less for treating home patients and requiring patient copays for home dialysis equipment and supplies. When Congress considered eliminating these disincentives, lobbyists for a large dialysis company shared inaccurate data to make home dialysis appear less safe than in-center dialysis and claimed that Drs. Scribner and Blagg lied about the benefits of home dialysis. Based on that, Congress did not change the disincentives for home dialysis and Medicare continued to pay more for in-center HD. With financial incentives favoring in-center HD, dialysis clinics popped up everywhere, many of which didn’t offer any type of home dialysis and most of which are for-profit now, with fewer non-profit or hospital-based clinics. We can do better.
Kidney disease is more common among minorities, who may have lower income, are more likely to have diabetes and/or high blood pressure, yet may have less access to healthcare and live in neighborhoods where fast food is plentiful and access to grocery stores with healthy food is less available. Mueller cited research showing that African Americans are more likely to be treated in lower rated clinics, to be hospitalized more, to not be offered home dialysis, to be slower being waitlisted for transplant and to get a transplant less often than white patients. He pointed out that until 2021 the eGFR calculator over-estimated kidney function in African American which delayed access to dialysis and transplant. We can do better.

Mueller wrote how internationally recognized Australian nephrologist Dr. John Agar and most other nephrologists believe dialysis sessions should be individualized to the patient instead of “cookie cutter.” They believe sessions should be long enough to avoid what Agar calls “bazooka dialysis.” Research shows that delivering dialysis with high ultrafiltration rates stuns organs, kills residual kidney function, and causes patients to have such symptoms as cramping, fainting, and feeling drained for several hours after dialysis.

Mueller interviewed many staff who were stretched thin caring for too many patients while required to do multiple tasks in a short time. They had poor morale, little patience, and shortened tempers. The combination of patients feeling bad emotionally and physically and staff feeling overwhelmed creates a tinder box for conflict. Speaking of conflict, Mueller spoke with hundreds of patients about their dialysis care and with Arlene Mullin who has served as a patient advocate for years and connects patients who complain about their care at clinics or face involuntary discharge (IVD) with pro bono attorneys. Mullin told Mueller about cases that might have been retribution for having filed complaints or written letters to elected officials complaining about their care. Meanwhile, patients told Mueller they hadn’t done what their records accused them of doing. The book included contents of a staff member’s letter in which she said her manager pushed her to falsify a patient’s records to justify involuntary discharge. Mullin said this was not uncommon—which is shocking. Mullin told him that most of those who contact her are people of color.
Mueller also quoted a well-known Canadian nephrologist who related a conversation with a U.S. nephrologist who described how he triggered a patient’s behavior to justify terminating his dialysis care. Another nephrologist told Mueller that he’d observed staff exaggerating evidence in patient records to support involuntary discharge. Mueller wrote that this happens more with Medicare and Medicaid patients and less with commercially insured patients—since those plans pay more. He quoted a commercially insured patient’s spouse who said after she questioned high bills for dialysis the clinic built a case with false “facts” that led to her husband’s discharge. He wrote—and I’ve observed when I’ve tried to advocate for patients—that those who are discharged are often blackballed and can’t find another doctor or dialysis clinic willing to admit them within long distances from their home. Those who can’t find another clinic must get care at hospitals, and may only get that care when their labs indicate they need dialysis emergently. This costs Medicare, Medicaid and other payers more. Involuntary discharge from dialysis is unique to the U.S. It doesn’t happen elsewhere. Mueller couldn’t find U.S. data on involuntary discharges, but the ESRD Networks track these data. In 2020, 663 patients were at risk of losing their access to care.3 Of the 400 patients who got 30-day letters threatening IVD, Networks averted 27 and found another clinic for 106. What happened to the other 267 patients? We can do better.

About profit-driven healthcare, Mueller describes several instances of how chasing profits led dialysis companies to take actions that led to government fines, and cites specific cases in the Epilogue and Annotations—Gambo paid over $350 million for civil and criminal allegations of Medicare fraud, for example. DaVita and subsidiaries paid $1.5 billion. Fresenius paid $231 million in a bribery case and $250 million to settle more than 10,000 GranuFlo lawsuits. Mueller pointed out that non-dialysis providers have been fined and CEOs have even gone to jail for greed-based actions. If dialysis companies can pay that much money in fines, it seems they could pay more to provide optimal care and staffing. We can do better.
Mueller wrote that outcomes are better in nonprofit clinics than in for-profit ones. This point has been disputed by for-profit providers. However, I found several additional articles published after he stopped writing that support what he wrote:
One reported the odds of dying were 7% higher in a for-profit clinic than in a not-for-profit clinic.4
Another found adult patients in for-profit clinics were less likely to be placed on a transplant waiting list, to receive a living donor transplant, or to receive a deceased donor transplant compared to patients in nonprofit clinics. After a coding error was corrected and the data re-analyzed, for-profit clinics had 2.6% fewer patients listed for transplant, 0.9% fewer living donor transplants, and 1.4% fewer deceased donor transplants.5
A study of pediatric patients found that those at for-profit clinics were less likely to be waitlisted or receive a living or deceased donor transplant. Differences were greater when pediatric patients were treated at a freestanding clinic. The authors stated most pediatric nephrologists treat patients in hospital-based clinics, not freestanding ones.6
Another study found that the pediatric patients’ risk of death was twice as high when they were treated at for-profit dialysis clinics compared to those treated at nonprofit clinics. Improving children’s access to transplant at for-profit dialysis clinics could reduce that risk.7
Again, we can and must do better.
These are just some things Tom Mueller wrote about in his book. In the last chapter, he cautions that many of the problems relate to what he calls “loss of homeostasis.” In his opinion, we have accepted too much for too long. There are those who will say that the book exaggerates and that things he reports don’t happen. Maybe they don’t in some/most clinics, but even if they happen in a few clinics, we can do better.
Blagg C. From Miracle to Mainstream: creating the world’s first dialysis organization: Early years of Northwest Kidney Centers. Seattle, WA: Northwest Kidney Centers, 2017.↩︎
Schatell D. As Nancy Spaeth’s Earthly Journey Ends, Her Inspiration Lives On. January 20, 2022.↩︎
End-Stage Renal Disease Network Program Summary Annual Report↩︎
Dickman S, Mirza R, Kandi M, Incze MA, Dodbiba L, Yameen R, Agarwal A, Zhang Y, Kamran R, Couban R, Guyatt G, Hanna S. Mortality at For-Profit Versus Not-For-Profit Hemodialysis Centers: A Systematic Review and Meta-analysis. Int J Health Serv. 2021 Jul;51(3):371-378↩︎
Gander JC, Zhang X, Ross K, Wilk AS, McPherson L, Browne T, Pastan SO, Walker E, Wang Z, Patzer RE. Notice of Retraction and Replacement. Gander et al. Association Between Dialysis Facility Ownership and Access to Kidney Transplantation. JAMA. 2019;322(10):957-973. JAMA. 2020 Apr 21;323(15):1509-1510. ↩︎
Amaral S, McCulloch CE, Lin F, Grimes BA, Furth S, Warady B, Brunson C, Siyahian S, Ku E. Association Between Dialysis Facility Ownership and Access to the Waiting List and Transplant in Pediatric Patients With End-stage Kidney Disease in the US. JAMA. 2022 Aug 2;328(5):451-459.↩︎
Ku E, McCulloch CE, Bicki A, et al. Association Between Dialysis Facility Ownership and Mortality Risk in Children With Kidney Failure. JAMA Pediatr. Published online September 05, 2023. doi:10.1001/jamapediatrics.2023.3414↩︎


Comments
Leong Seng Chen
Oct 14, 2023 3:55 AM
Susan G Emeny
Sep 24, 2023 11:02 AM