Gentle UF Benefits ALL Hemodialysis patients

“2 hours into treatment I get full body muscle cramps/convulsions and feel like I'm dying.”
At MEI, ever since we learned in 1997 that health-related quality of life (HRQOL) in people with end-stage kidney disease predicts hospitalization and death, we’ve been huge proponents of this self-reported measure that brings the patient’s voice into dialysis care.1,2 We even built a tool to help clinics use the data for patients’ care plans.
Last month, a study found that intradialytic hypotension (IDH; BP crashes during HD) significantly reduced HRQOL.3 IDH occurred 11.1% of the time in data from 17,892 HD sessions (n=497). The more frequent the IDH, the worse HRQOL scores were. The most recent paper I could find estimating IDH prevalence in the U.S. was 2014—and the rate was 35.5% higher than in the new study, with large per-patient variations.4 “But, everyone defines IDH differently!” you might say, and it’s true. (It’s also true that we need better, recent data on this potentially lethal problem.)
The Main Mechanism of IDH Harm is Stunning

IDH starves organs of oxygen during HD treatments—which can stun the heart (myocardial stun), brain, any residual kidney function, and the gut—increasing mortality.5 Why does blood pressure drop? It’s a complex issue, and Davenport suggests these reasons:
Patient age, comorbidities, dietary compliance
Reactions to the extracorporeal circuit and medications
Choice of dialysate composition and temperature
Setting of postdialysis target weight
Ultrafiltration rate and profiling
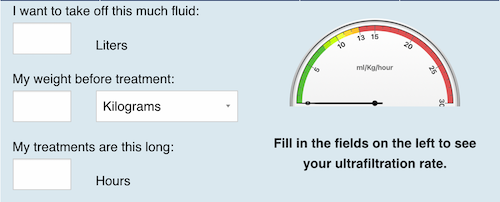
Ultrafiltration rate was the target of a 2014 consensus document signed by the Chief Medical Officers of US dialysis providers, who felt strongly that in-center HD could—and should—be done better, and they made three recommendations:6
Make extracellular fluid status a component of sufficient HD—vs. “the lowest achieved weight before a patient ends up in the Trendelenburg position.”
Remove fluid gradually. “UFR>10 mL/h/kg was associated with significantly increased risk of intradialytic hypotension and all-cause mortality.”
Avoid sodium loading at dialysis. “Patients therefore frequently would undergo dialysis against a dialysate that may result in net diffusive movement of sodium into the patient…”
Eleven years later, sodium modeling is, happily, virtually gone from in-center HD. But incorporating extracellular fluid status into a definition of “sufficient HD”? Nope. Gradual fluid removal? Not so much. The latter is, however, easily achieved with home HD. (You knew I’d fit that in here somewhere, right?)
An Idea to Connect Some Dots • • • • • • • •
ASN just released brand new, hot-off-the-presses guidance on Outpatient management of patients with dialysis-requiring acute kidney injury,7 which appropriately focuses on providing personalized dialysis to increase the chance of recovery of kidney function (currently estimated at 31%). But, maintaining residual kidney function (RKF) also predicts survival in people with end-stage kidney disease in whom recovery of function is not expected. Analysis of more than 39,000 patients revealed a significant (p < 0.05) trend toward higher mortality with lower RKF, and loss of RKF.8 In the BISTRO trial, “Lower RKF during the first 2 years of hemodialysis is associated with an increased death risk for up to 50 months after dialysis initiation.”9
Perhaps rather than focus the individualized and intensive focus on RKF protection solely on patients with AKI, wouldn’t it save lives—and dollars— to also extend this care to incident HD patients with ESKD who have residual kidney function to protect? Or, of course, to help more patients choose a home therapy that is less likely to cause IDH?
DeOreo P. Hemodialysis patient-assessed functional health status predicts continued survival, hospitalization, and dialysis-attendance compliance. Am J Kidney Dis. 1997 Aug;30(2):204-212↩︎
Lowrie EG, Curtin RB, LePain N, Schatell D. Medical outcomes study short form-36: a consistent and powerful predictor of morbidity and mortality of dialysis patients. Am J Kidney Dis. 2003 Jun;41(6):1286-92. Doi: 10.1016/s0272-6386(03)00361-5↩︎
Zhi M, Zeng Y, Chen C, Deng S, Liu Y, Huang Y, Chu B, Hu H. The relationship between intradialytic hypotension and health-related quality of life in patients undergoing hemodialysis: a cross-sectional study. Sci Rep. 2025 Apr 4;15(1):11532. Doi: 10.1038/s41498-025-96286-y↩︎
Sands JJ, Usvyat LA, Sullivan T, Segal JH, Zabetakis P, Kotanko P, Maddux FW, Diaz-Buxo JA. Intradialytic hypotension: frequency, sources of variation and correlation with clinical outcome. Hemodial Int. 2014 Apr;18(2):415-422. Doi: 10.1111/hdi.12138↩︎
Davenport A. Why is intradialytic hypotension the commonest complication of outpatient dialysis treatment? Kidney Int Rep. 2022 Nov 10;8(3):05-418. Doi: 10.1016/j.ekir.2022.10.031↩︎
Weiner DE, Brunelli SM, Hunt A, Schiller B, Glassock R, Maddux FW, Johnson D, Parker T, Nissenson A. Improving clinical outcomes among hemodialysis patients: a proposal for a “volume first” approach from the chief medical officers of US dialysis providers. Am J Kidney Dis. 2014 Nov;64(5):685-95. Doi: 10.1053/j.ajkd.2014.07.003↩︎
Vijayan A, Heung M, Awdishu L, Babroudi S, Green GB, Koester L, McCoy IE, Menon S, Palevsky PM, Proctor LA, Selewski DT, Struthers SA, for the ASN Kidney Health Guidance Workgroup on Outpatient Dialysis for AKI. ASN kidney health guidance on the outpatient management of patients with dialysis-requiring acute kidney injury. J Am Soc Nephrol. 2025 May 1;36(5):926-939. Doi: 10.1681/ASN.0000000646↩︎
Okazaki M, Obi Y, Shafi T, Rhee CM, Kovesdy CP, Kalantar-Zadeh K. Residual kidney function and cause-specific mortality among incident hemodialysis patients. Kidney Int Rep. 2023 Aug 3;8(10):1989-2000. Doi: 10.1016/j.ekir.2023.07.020↩︎
Belcher J, Coyle D, Lindley EJ, Keane D, Caskey FJ, Dasgupta I, Davenport A, Farrington K, Mitra S, Ormandy P, Wilkie M, Macdonald J, Solis-Trapala I, Sim J, Davies SJ. Impact of the preservation of residual kidney function on hemodialysis survival. Results from the BISTRO Trial. Kidney360. 2025 Jan 1;6(1):112-120. Doi: 10.34067/KID.0000000596↩︎


Comments