2026 Medicare Advantage Open Enrollment Ends on March 31

People who have Medicare Advantage plans can switch from one MA plan to another from January 1 through March 31 annually. Their new plan will start the first day of the next month. Those who have an MA plan can switch to Original Medicare and buy a stand-alone Part D plan then too. However, if they have had the MA plan for longer than one year, they may not be able to get a Medigap (Medicare supplement) plan to help pay Original Medicare’s deductibles, copays, and coinsurance. There are other times when those who are eligible for Medicare can join or switch health plans including October 15-December 7 each year and other dates if they qualify for a “special enrollment period” (SEP) because they moved, were released from jail/prison, or lost their coverage.1
Types of Medicare Advantage (MA) plans
The Medicare website allows people to review and compare different types of Medicare Advantage plans.2
Health Maintenance Organizations (HMOs), pay only for in-network providers except in an emergency, out-of-area urgent care, or out-of-area dialysis
Preferred Provider Organizations (PPOs), pay for in- and out-of-network, less for out-of-network
Special Needs Plans, one type is Chronic Disease including ESRD (not widely available)
Medicare Savings Accounts, combine a high-deductible plan with a medical savings account that is used to pay providers
Private Fee-for-Service (PFFS) plans, pay for any provider that accepts Medicare, with no referrals needed to see specialists, but the PFFS decides what patient will pay; it can’t be more for dialysis
A chart compares premiums, drugs, choice of providers, whether a primary care doctor is needed, and if a referral is needed to see a specialist for all these types of MA plans. The site also has a link to the plan finder to see more detailed information about plans sold in a specific area along with their cost, coverage, and plan documents.3
MA Plan Cost, Coverage, and Provider Networks from Year to Year
Have you heard patients complain that their MA plan isn’t paying for things as they expected? Are they having issues with higher than expected out-of-pocket costs or preferred providers being out of network? Unfortunately, despite multiple TV ads and mailings, some patients assume that the plan they had last year will be the same this year or don’t have the time, energy, or understanding to research plans as they are encouraged and advised to do. This can be devastating EXCEPT that people with an MA plan can switch to a different MA plan from January through March every year. Patients can also switch from an MA plan to Original Medicare, but unless the patient can also get a Medigap (Medicare supplement) plan to help to pay Medicare’s out-of-pocket costs, they would have to pay Medicare Part A and B deductibles, copays and coinsurance. The state health insurance assistance program (SHIP) is a great resource. Counselors are CMS-trained, unbiased, and merely counseling vs. selling, and can help people review their options. When reviewing plans with an insurance broker be aware that they may only sell certain plans, and they get incentives for making a sale. You can look up SHIP contacts by state.4
Home Dialysis Patients with MA Plans
The United States Renal Data System, reported the percentage of new and established home dialysis patients who had an MA plan in 2023.5
| Incident patients | Home HD | PD |
|---|---|---|
| Medicare Advantage | 9.3% | 10.0% |
| Medicare Advantage/Medicaid | 1.2% | 1.0% |
| Prevalent patients | Home HD | PD |
|---|---|---|
| Medicare Advantage | 17.1% | 21.2% |
| Medicare Advantage/Medicaid | 13.0% | 11.4% |
Advantages and Disadvantages of MA Plans
The National Council on Aging provides information on the pros and cons of MA plans.6
| Advantages | Disadvantages | |
|---|---|---|
| Costs | In 2026, after paying a Part B premium of $202.90, MA plan premiums average $14/month and may be less. The cap on Part A & B services is $9,250 and may be less; drugs are not included under this cap. Costs can include deductibles, copays, and coinsurance as in employer plans. Those with Medicaid and/or a Medicare Savings Program may get help for costs. | Copays are due before a patient gets a service and if there are multiple visits, copays can be high. Original Medicare has no cap, but if a patient can get a Medigap plan, the most s/he will pay for Medicare-covered services is $283 (the Part B deductible). People with MA plans cannot get a Medigap plan. |
| Coverage | Includes Part A & B services. Most include Part D, or members can buy a separate Part D plan. May cover benefits Original Medicare doesn’t (dental, vision, hearing, wellness, limited nutrition, transportation, etc.). There may be a premium for extra benefits. | With MA, HMO provider choice is limited to those in the plan’s directory. With an MA PPO, out of network providers cost more. As with stand-alone Part D plans, drugs are limited to those on the plan’s formulary. To limit costs, plans may require prior authorization, which requires a doctor’s medical justification to get the plan to pay for surgery, hospital stays, home health, medical equipment, etc. |
| Access to providers | A primary doctor acts as a “gatekeeper.” Patients may need referrals to see a specialists. A gatekeeper may help coordinate care. | There is no gatekeeper for people with Original Medicare who can see any provider that accepts Medicare. So, they have greater freedom of choice, but may have less care coordination. |
Medicare Advantage Plans in the U.S.7
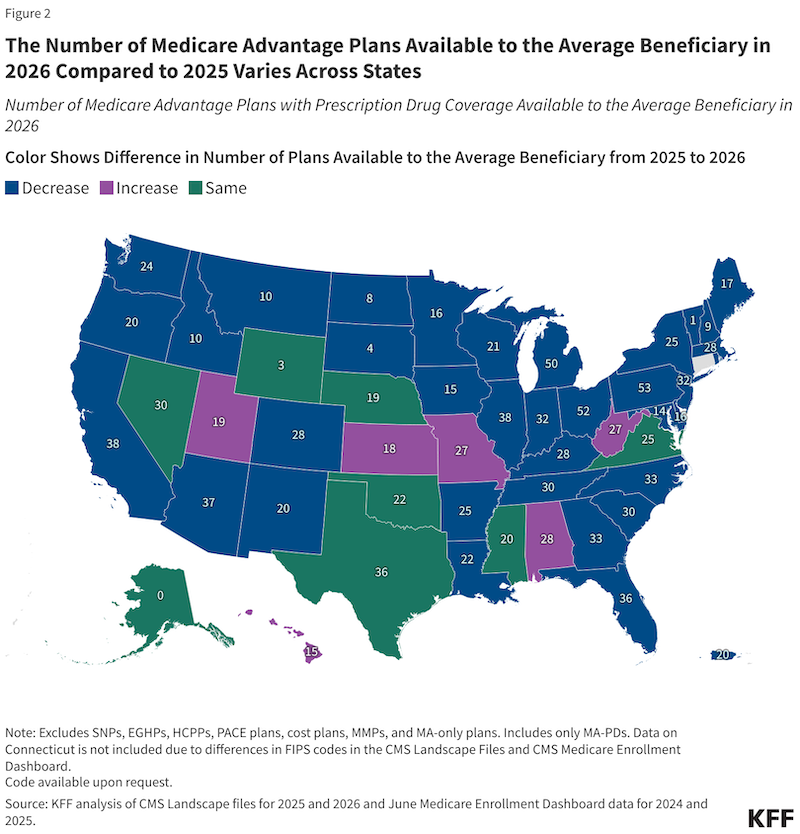
KFF provides this map showing how many plans were available in 2026 compared to 2025.
Number of Members in MA Plans
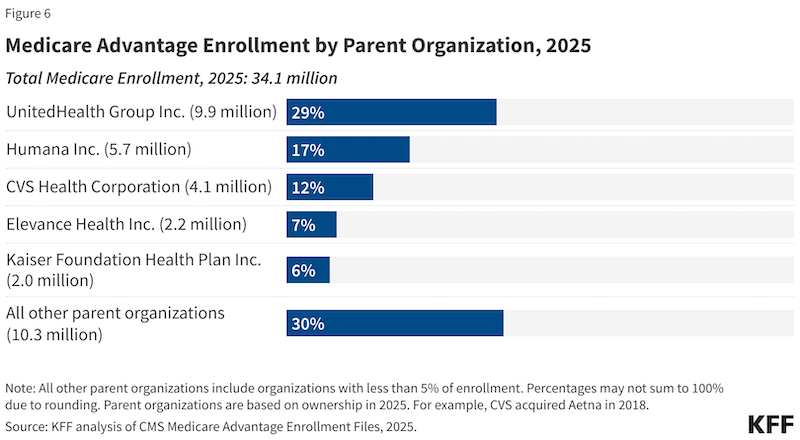
KFF reported that UnitedHealth Group and Humana had about 46% of all MA plan members in 2025. Other plans’ members make up the rest.8
Plan Denials & Appeals
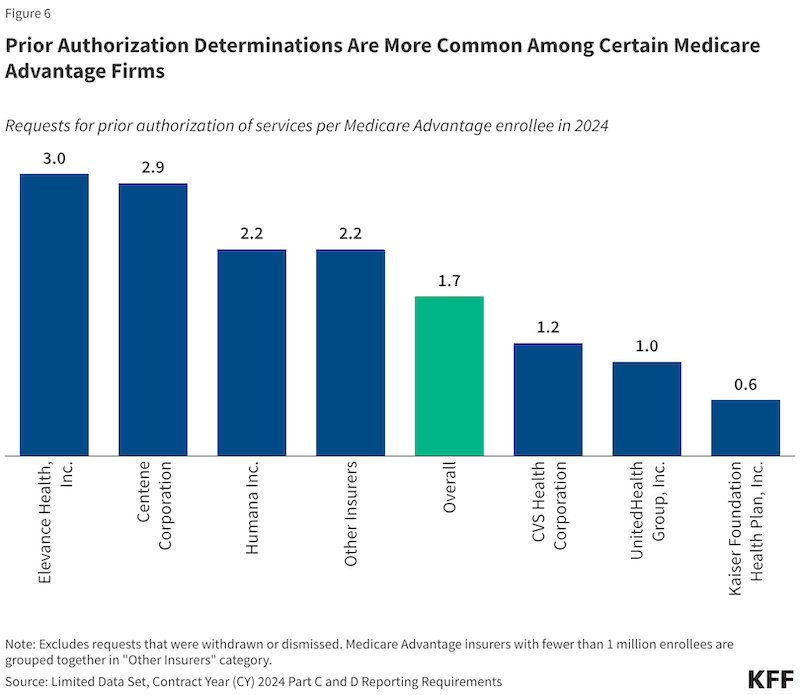
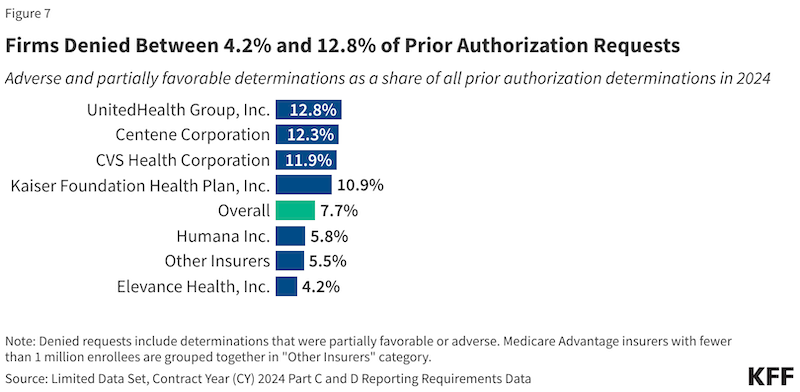
A concern that has been raised about MA plans is the requirement for prior authorizations (PAs)—common for hospitalizations, nursing home stays, and chemotherapy—and the high number of full or partial PA denials. A KFF report9 provided data that showed that in 2024, MA plans reviewed 53 million prior authorization requests and denied 4.1 million (7.7%). Only 11.5% of PA denials were appealed. Of those appeals, 80.7% were then partially or fully approved. Elevance and Centene plans had the highest percentage of requests per enrollee whereas UnitedHealthcare and Humana, which together had 46% of the number of members in MA plans had the lowest number of requests per enrollee.
Conclusion
MA plans advertise heavily during enrollment periods—focusing on the benefits and failing to mention the downsides. Patients considering joining or switching to a Medicare Advantage plan may rely on brokers or a company’s customer service staff to inform them about the plan. If they do not feel confident or do not have the time to fully investigate plan contract, provider network, and drug formulary, a state health insurance assistance program (SHIP) counselor can help for free through one-on-one counseling by phone or in-person. Choosing the wrong plan can be a costly mistake and require changes in trusted providers.
Medicare.gov. Joining a plan. https://www.medicare.gov/basics/get-started-with-medicare/get-more-coverage/joining-a-plan↩︎
Medicare.gov. Your health plan options. https://www.medicare.gov/health-drug-plans/health-plans/your-health-plan-options↩︎
Medicare.gov. Compare Type of Medicare Advantage Plans. https://www.medicare.gov/health-drug-plans/health-plans/your-health-plan-options/compare↩︎
State Health Insurance Assistance Programs (SHIPs) help you navigate the complexities of Medicare. https://www.shiphelp.org/what-we-do/↩︎
United States Renal Data System. 2025 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2025. https://usrds-adr.niddk.nih.gov/2025/end-stage-renal-disease/1-incidence-and-prevalence↩︎
National Council on Aging. Weighing the Pros and Cons of Medicare Advantage. December 3, 2025. https://www.ncoa.org/article/weighing-the-pros-and-cons-of-medicare-advantage/↩︎
Freed M, Biniek J, Ochieng N, Damico A, Neuman T. KFF. Medicare Advantage 2026 Spotlight: A First Look at Plan Offerings. December 9, 2025. https://www.kff.org/medicare/medicare-advantage-2026-spotlight-a-first-look-at-plan-offerings/↩︎
Ochieng N, Freed M, Biniek JF, Damico, Neuman T. KFF. Medicare Advantage in 2025: Enrollment Update and Key Trends. July 28, 2025. https://www.kff.org/medicare/medicare-advantage-enrollment-update-and-key-trends/↩︎
Biniek JF, Sroczynski N, Freed M, Neuman T. KFF. Medicare Advantage Insurers Made Nearly 53 Million Prior Authorization Determinations in 2024. January 28, 2026. https://www.kff.org/medicare/medicare-advantage-insure↩︎


Comments