How to Talk to Patients About Home Dialysis: Four Steps for Professionals
You have a patient who will soon need dialysis. Or, an in-center hemodialysis (HD) patient seems like a good candidate for home. What is the best way to discuss treatment options, and what should you say? This guide will help make that challenging conversation easier—even if you don't have any experience with home treatments.
Times are Changing
In 1972 when President Nixon signed Public Law 92-603 to create the Medicare ESRD Program, about 40% of patients dialyzed at home.1 By 2009, just 8.9% did.2 Our 2010 nephrologist survey found that even though 92% of U.S. patients were on standard in-center hemodialysis (HD)—just 6% would choose it for themselves if their own kidneys failed.3 This was quite a disconnect!
After the Executive Order on Advancing American Kidney Health took effect in 2019, Medicare developed payment models to promote home dialysis, like the ESRD Treatment Choices (ETC) Model, now mandatory for 30% of U.S. dialysis clinics. Those that meet targets to increase use of home treatments will get payment incentives. The goal for home dialysis is at least 19% of eligible patients by the end of 2027.4 This is why it will help you and your clinic to know how best to approach patients—and how not to. Here are the steps we recommend.
Step 1: Address the Storm of Emotions
MEI did some of the first research talking with dialysis patients about how they felt. What came through loud and clear were their emotions:
-
Anger: with themselves, doctors who missed a diagnosis, God.
-
Depression: their new lives were not what they expected.
-
Fear and Anxiety: they all feared dying—or a life not worth living.
Importantly, almost no one told their care teams of their worries. Some made poor choices in the grip of fear—like the college student who broke off her engagement and got her tubes tied, believing she could not marry or become a mother. Or, the man who never bought a home, since he would not live long enough to pay off a mortgage. (Do any of us know that we will?)
Since then, we have answered the “How long can you live?” and “How well can you live?” questions proactively in our materials—even if patients never ask out loud. What we share with you here is informed by more than 20,000 kidney patients over 30+ years.
Education is key to modality choice. But, we humans cannot learn when we are afraid.5 When stress hormones (cortisol, adrenaline) course through our veins, we can fight. We can flee. We can freeze. But, we can't form new memories.
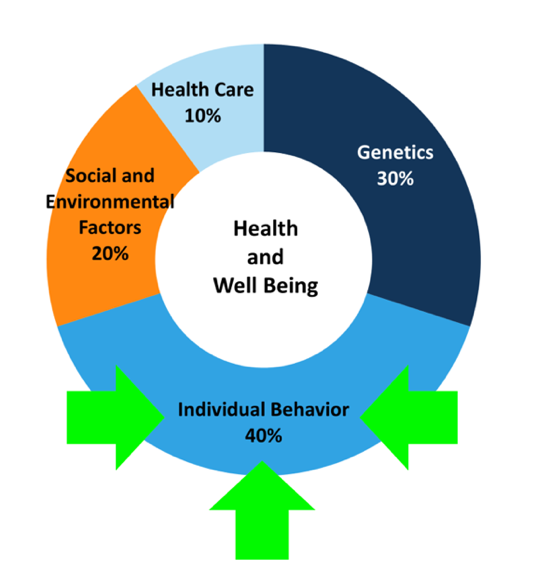
Education at this point is wasted: your patients cannot hear you and will not recall what you say. Yet, 40% of key health outcomes are driven by patient behavior.6 We must engage patients in their own care and healthcare decisions. To succeed, we have to help them get past fear.
What You Can Do: Normalize Patients' Feelings
Help them see that they are not alone and that how they feel is expected. Sit down. Put a hand on their arm or shoulder. Say something like:
“I know this must be scary for you.”
“What questions can I answer?”
Find out what they know—or believe—so myths can be addressed. Acknowledge patients' fears or find someone who can, like the social worker. A patient mentor can help, as patients often want to know what their fellows think.
Step 2: Offer Hope for a Good Life
What gets people past fear? Hope. Hope and fear are “two sides of the same coin,” found authors of a meta-analysis.7 Studies have found that hopeful kidney patients:
Slowed CKD progression and reduced the risk of fast kidney decline.8
Were less depressed, anxious, and stressed.9
Had better mental functioning.10 This predicts fewer hospital stays and deaths.11
Felt less burdened by diet and fluid limits and had lower blood pressure.15
Gained less fluid weight, missed fewer sessions, and followed potassium limits.16

Hope looks like life before kidney disease. We may know that people are lucky to have options to live past kidney failure. Yet, each option can affect every aspect of life—work, travel, intimacy, pets, energy level, sleep… A poor fit can threaten everything that matters to someone. Like chemo or radiation for cancer, all of the choices look bad: patients don't want to need any of them.
For this reason, we do not recommend saying things like, “You would do great on PD!” or “Have you thought about home dialysis?” A modality-first approach like this assumes that patients are as enthusiastic about home treatments as we may be. But, to paraphrase Joan Lunden, “People have to want something more than they are afraid of it.” And, our patients are very afraid.
Instead, our job is to help them reframe the options in terms of what they do want: full, vibrant lives. How? Use our evidence-based decision aid that does the work for you (see the blue box). Say something like:
“I have a tool that can help you figure out how to have the life you want.”
“Let me help you get started.”
What You Can Do: Use My Life, My Dialysis Choice
This free MEI tool in English and Spanish is written at a 5th grade level, designed to offer hope, and starts with patients' values. It maps values onto dialysis options—so you don't have to—and has been extensively tested and adopted by a large dialysis organization. Start options education here. Use a large tablet. Ask patients to choose their top 3 values.
For each value, the tool will display a page that explains the value and has seven dialysis options in four boxes. Each box contains pros and cons for that value. The patient rates each box with 0-4 stars. Each value will take about 5 minutes. Some patients will need help to use the tablet.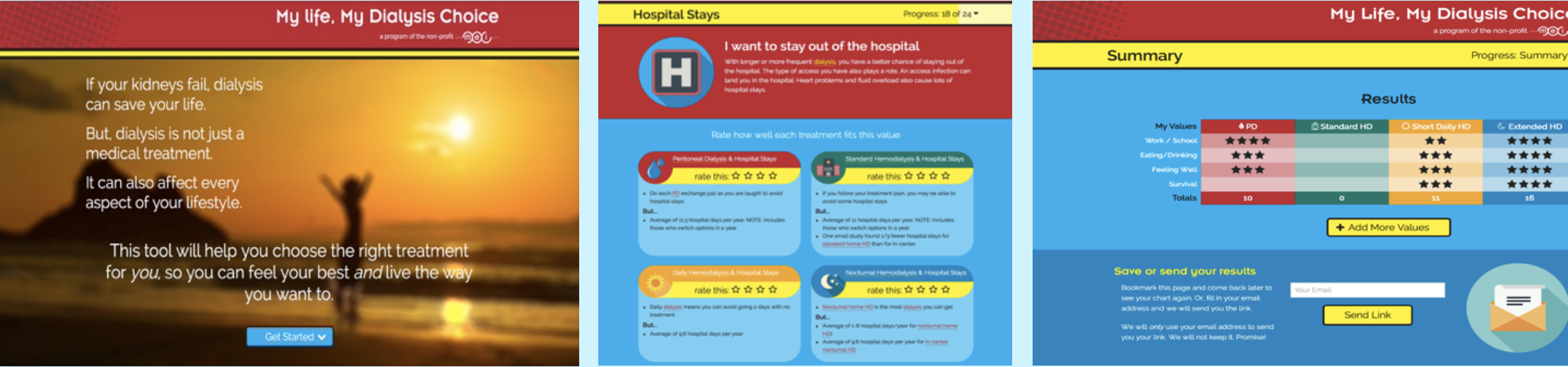
Once done, the tool creates a 1-page summary of a patient's values and star ratings. This can be printed as part of the medical record, and serves as a Plan of Care for modality choice.
Try it yourself! Your choice of treatment option might surprise you. NOTE: Watch for an update, coming soon, with a new name and a new look. It will include transplant and comfort care. Once it is live, you will see it when you go to My Life, My Dialysis Choice.
Step 3: See if Patients Can Do the Treatment(s) They Prefer
My Life, My Dialysis Choice can help patients and clinicians communicate for shared decision-making. It cannot assess whether patient choices will suit their anatomy, mental health, or living situation. For example, about 87% of people may be physically suited for PD;17 the rest are not.
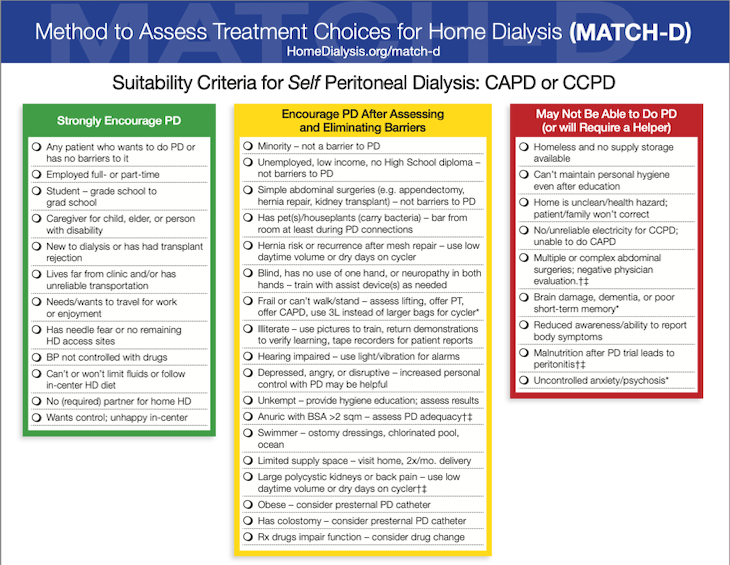
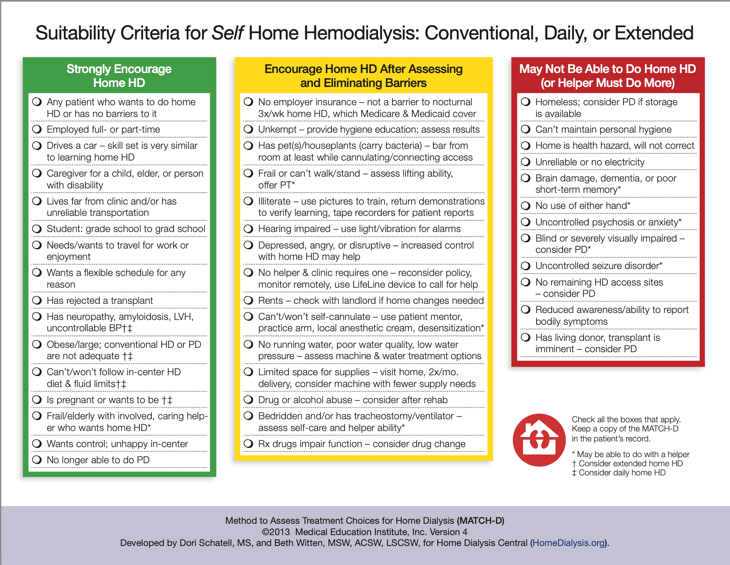
What You Can Do: Use our free Method to Assess Treatment Choices for Home Dialysis (MATCH-D) for PD and home HD.
The MATCH-D levels the playing field to help remove implicit and explicit bias and ensure that all patients are treated fairly. It will help you determine who may be excellent candidates for PD or home HD, who may have challenges that can be overcome, and who would need help to dialyze at home.
Step 4: Refer the Patient for Options Education
Once people have their goal in place—a desire to keep what matters most in their lives—they will be more hopeful and open to education. Now, you can ask them to attend a class or a one-on-one education session to learn more of the details of the option(s) they are willing to consider.
What You Can Do: Send Patients to a Local Class—Or Offer Your Own
Live classes are terrific, especially when members of the care team, including the home training nurse if your clinic has one, and patients using different options can be included. In these COVID days, classes may have to be held online, which can still work well for those with a smartphone or computer access.
No class in your area? Use our free How to Have a Good Future with Kidney Disease slide toolkit or videos. After education, talk to them, see what their choice is, and help them get started.
Conclusion
The steps to help patients understand their treatment options are:
Address—and normalize—the storm of emotions.
Offer patients hope for a good life.
See if patients can do the treatments they are interested in.
Refer patients for options education.
Selected Resources & Tools
Home Dialysis Central - www.homedialysis.org
Home Dialysis Central Facebook Discussion Group (Private group, ) - www.facebook.com/groups/HomeDialysisCentral
Kidney School (18 modules English/Spanish, print, audio) – www.kidneyschool.org
Life Options – www.lifeoptions.org
Partner Agreement on Tasks for Home Dialysis (PATH-D) – PD and home HD. www.homedialysis.org/professional-tools/path-d
Teaching Resources – www.lifeoptions.org/resources-for-professionals/#teaching-resources
References:
Blagg CR. A brief history of home hemodialysis. Adv Ren Replace Ther. 1996 Apr;3(2):99-105↩︎
Qamar M, Bender F, Rault R, Piraino B. The United States' perspectives on home dialysis. Adv Chronic Kidney Dis. 2009 May;16(3):189-97↩︎
Merighi JR, Schatell DR, Bragg-Gresham JL, Witten B, Mehrotra R. Insights into nephrologist training, clinical practice, and dialysis choice. Hemodial Int. 2012 Apr;16(2):242-51↩︎
Medicare Program; Specialty Care Models To Improve Quality of Care and Reduce Expenditures. Centers for Medicare & Medicaid Services. 85 Fed. Reg. 61353 (September 29, 2020), 42 CFR 512.↩︎
Lindstrom BR, Bohlin G. Threat-relevance impairs executive functions: negative impact on working memory and response inhibition. Emotion. 2012;12(2):384-393↩︎
Schroeder SA. Shattuck lecture. We can do better—improving the health of the American people. N Engl J Med. 2007 Sep 20;357(12):1221-1228↩︎
Hammer K, Mogensen O, Hall EOC. The meaning of hope in nursing research: a meta-synthesis. Scand J Caring Sci. 2009;23;549-557↩︎
Glover LM, Butler C, Cain-Shields L, Forde AT, Purnell TS, Young B, Sims M. Optimism is associated with chronic kidney disease and rapid kidney function decline among African Americans in the Jackson Heart Study. J Psychosom Res. 2020 Dec;139:110267↩︎
Rahimipour M, Shahgholian N, Yazdani M. Effect of hope therapy on depression, anxiety, and stress among the patients undergoing hemodialysis. Iran J Nurs Midwif Res. 2015 Nov-Dec;20(6):694-699↩︎
Billington E, Simpson J, Unwin J, Bray D, Giles D. Does hope predict adjustment to end-stage renal failure and consequent dialysis? Br J Health Psychol. 2008 Nov;13(Pt 4):683-99↩︎
Lowry EG, Curtin RB, LePain N, Schatell D. Medical Outcomes Study Short Form-36: a consistent and powerful predictor of morbidity and mortality in dialysis patients. Am J Kidney Dis. 2003 Jun;41(6):1286-1292↩︎
Alshraifeen A, Al-Rawashdeh S, Herth K, Alnuaimi K, Alzoubi F, Khraim F, Ashour A. The association between hope and quality of life in haemodialysis patients. Br J Nurs. 2020 Nov 26;29(21):1260-1265↩︎
Al-Rawashdeh S, Alshraifeen A, Rababa M, Ashour A. Hope predicted quality of life in dyads of community-dwelling patients receiving hemodialysis and their family caregivers. Qual Life Res. 2020 Jan;29(1):81-89↩︎
Sajadi SA, Farsi Z, Akbari R, Sadeghi A, Pasha AA. Investigating the relationship between quality of life and hope in family caregivers of hemodialysis patients and related factors. BMC Nephrol. 2021 22:383↩︎
Kurita N, Wakita T, Ishibashi Y, Fujimoto S, Yazawa M, Suzuki T, Koitabashi K, Yanagi M, Kawarazaki H, Green J, Fukuhara S, Shibagaki Y. Association between health-related hope and adherence to prescribed treatment in CKD patients: multicenter cross-sectional study. BMC Nephrol. 2020 21:453↩︎
Ghahfarokhi MM, Mommadian S, Nezhad BM, Kiarsi M. Relationship between spiritual health and hope by dietary adherence in haemodialysis patients in 2018. Nurs Open. 2019 Dec 11;7(2):503-511↩︎
Mendelssohn DC, Mujais SK, Soroka SD et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol Dial Transplant. 2009 24:555-61↩︎

