What You Need to Know About Sepsis

Did you know that each year in the U.S., about 350,000 people die from sepsis? It is the third leading cause of death. People with chronic illness are at a higher risk. It goes almost without saying that people on dialysis are at a very high risk of sepsis and so, in the interest of saving lives, all patients should be aware of it. In case no one else has given you the run-down of this issue lately, here goes…
Sepsis is a system-wide body response to an infection. Any infection. A person can become deathly ill from a cold, a scrape, a break in sterile technique, or even a UTI.
For reasons that aren’t fully known, the immune system will sometimes over-work itself into chaos. This is how sepsis starts. Blood vessels leak, fluid shifts, and the body sends messages to bleed and clot—at the same time.
When it starts, sepsis looks and feels a lot like the onset of a very bad cold. Chills, shakes, aches, and fatigue. A rash may appear. Patients might have a fever—or they may be very cold.
Blood pressure drops, so organs get less oxygen. The heart beats fast and hard in a desperate attempt to get blood flow back to deep tissues. The rate of breath gets faster to try and balance pH in the body.
Per the Sepsis Alliance, the chance of survival at this point goes down by 8% per hour.

With blood pressure very low, the whole body is slowly dying. Without blood flow, organs begin to fail. As organs fail, the heart works itself into exhaustion trying to stop further damage. In time, it will stop. As tissue dies, wastes build up. The liver fails. The patient becomes confused as the brain is starved of oxygen. The nervous system is affected in the same way. The lungs tire, and fill up with fluid. Oxygen exchange grows even harder. The kidneys fail (or have already failed), limbs die off, and there is no easy way back to balance.
This is septic
shock. It is a mess, and 40% of the people who
get to this point do not live, not even with help.
An ICU will give lots of IV fluid to fill the vessels and give the heart
some pressure to beat against. They will treat or remove the source of
infection, if they can. They will give high doses of meds (“pressors”)
that cause blood vessels to tighten, to try and get any organ system
back on board. Oxygen, steroids, insulin, dialysis, ECMO, thoughts, and
prayers. It is hard road to get better from sepsis.
For those who live, there are often long-term issues to deal with: organ damage, PTSD, pain, fatigue, weakness, and more. Sepsis can shorten lives, and because of that, it is best to avoid it in the first place. Your best defense against sepsis is to know what to look for.
All adults should know if they are at risk for sepsis and when to worry about it. It might not even be your own life that you save with this knowledge; it could be a loved one. No one knows what is lurking right around the corner!
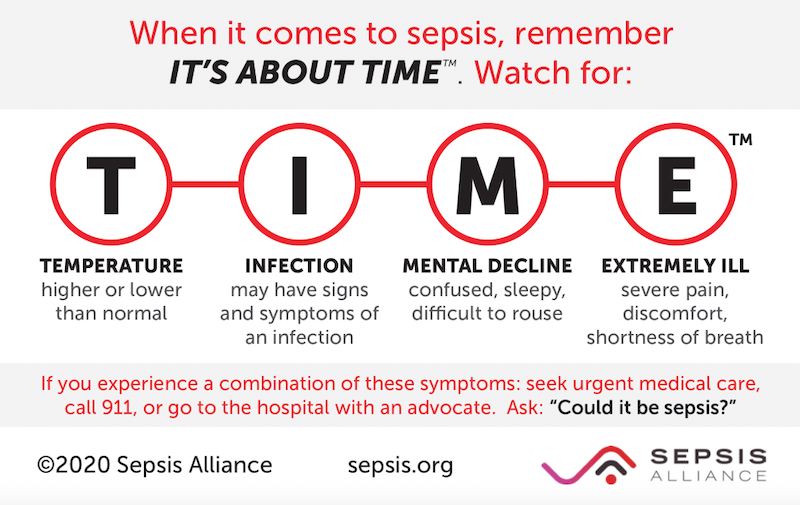
These are the signs of a major problem! If you have any of them, GET HELP NOW! Call 911. Go to the ER. Ask: “Could this be sepsis?” because that one simple question can remind staff that TIME is of the essence!
To prevent sepsis, good hand-washing and hygiene are the best lines of defense:
- Aseptic practice in medicine is a matter of life and death, and no one is without flaw. Speak up if you think staff needs a hand-scrub.
- Critique yourself at home and make changes to protect your body.
- Be sure to get your vaccines to prevent disease.
- Follow local rules for masking. You can always choose to wear a mask when out in crowds to reduce your risk.
- Good nutrition can lessen the chances of getting sepsis, too.
Again, know that you are your own best advocate! Being able to quickly notice problems is the best way to keep yourself safe. TIME matters in SEPSIS.
To learn more, visit the Sepsis Alliance at www.sepsis.org

