Sepsis Prevention Tips from a Survivor

September is Sepsis Awareness month. What a wonderful time to present or renew all the facts we should know to prevent, understand and cope with sepsis and post sepsis issues. I’ve been one of the very fortunate to have had sepsis seven times and survived. Each time has required weeks in hospital. According to Sepsis Alliance once you’ve had sepsis you’re at a higher risk of acquiring it again. I’ve beaten the odds so many times I feel like a walking miracle! Others I’ve known were not as lucky. One friend died when he couldn’t afford treatment for an infected molar. It quickly progressed to sepsis and could not be treated in time to save his life. One of my nurse’s father acquired pneumonia, was improperly diagnosed and sent home (with sepsis)—and died. Sadly, it happens.
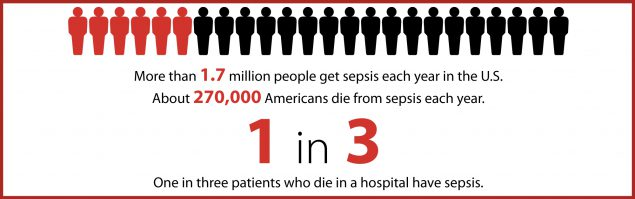
According to the CDC 1.7 million Americans acquire sepsis on a yearly basis and 270,000 die. One in three people who die in a hospital, die from sepsis.
SEPSIS is a body’s severe response to infection in the body. It can start out as a simple cut, bite, sore throat, flu, pneumonia, or from a recent surgery or procedure—and progress. Infection invades the bloodstream and the body attacks itself as a response. Without timely and proper treatment, sepsis can lead to organ failure, tissue damage and death. Yes, I said death! As many as 1/3 or 30% of those with sepsis don’t make it. That’s 30% who die. Do I have your attention yet?
Some other names for sepsis are:
Septicemia
Blood poisoning
Bloodstream infection (BSI)
Sepsis is life-threatening and not to be dismissed. Anyone can get an infection, and almost any infection can lead to sepsis, but some people are at a higher risk, including those:
With lower or weakened immune systems
Over age 65 or under age 1
With chronic health conditions such as diabetes, lung problems, cancer—or kidney disease.
Sepsis is not diagnosed simply on the basis of infection. The Sepsis Alliance shows signs to be aware of in a simple anagram: “When it comes to SEPSIS it’s about TIME.” Watch for:
T: Temperature that is higher—or lower—than normal.
I: Infection. May have signs or symptoms of infection.
M: Mental status. May be sleepy, confused, difficult to arouse.
E: Extremely ill. “I feel like I might die”
Other symptoms of sepsis may include: 1
Shortness of breath
High heart rate
Shivering or feeling very cold
Extreme pain or discomfort
Clammy or sweaty skin
Unusually low blood pressure
The symptoms can be vague, but if you have concerns about an infection, address them with your healthcare team. Ask “Could this infection be leading to sepsis?” A set of symptoms and bloodwork will likely confirm or rule out sepsis. These could include low oxygen levels in the blood, low urine output, organ failure (shown by blood tests) and more. Those who have these identifiers could have sepsis, which can progress to septic shock: the most severe level, diagnosed when your blood pressure drops to dangerous levels.
My First Sepsis Story
Let’s really talk about symptoms. I was using a newer graft in my arm, but due to continual stenosis (narrowing of the vessel) also had a chest catheter. A few days after an angioplasty (ballooning open the vessel), I began to just feel crummy: lethargic, just not up to my normal self. It started out with a low-grade fever, listlessness, uninterested in anything but generally irritated at everything. Vague? Absolutely. Then, it began to get worse. I saw my nephrologist, who told me, “It’s just *the crud*, give it time. You’ll get better.” I had no visible signs of infection either from my graft or my catheter. No redness, soreness, swelling or “hot” to the touch was visible.
The next day, within 15 minutes of starting my home hemodialysis treatment, I began to shiver uncontrollably. My temperature shot up to 103. My heart rate was 120 or higher and it felt like I couldn’t catch my breath. My hip hurt. The bone felt like it was on fire. We discontinued dialysis. I fought going to the ER. (We knew we couldn’t go to our local rural hospital as they were completely unfamiliar with dialysis, catheters etc. One ER doctor tried to tell me I didn’t understand the concept of hemodialysis and peritoneal dialysis and couldn’t possibly be doing home hemodialysis as it didn’t exist. So, our local ER was not an option.) Our best option was to go to the hospital where my nephrologist had privileges—110 miles away, in blizzard-like conditions.
I continued to shiver, have a fever, breathing fast, low blood pressure, fast heart rate and horrid pain. When you’ve had “shivers” for an extended period, your muscles begin to hurt. It’s an odd feeling. After a few hours, my husband and son had finally decided it was time to go. They put me in pajamas and slippers, wrapped me in a blanket, and carefully, slowly walked me to the car. Snow had accumulated to several inches. Our farm was several miles off blacktop, and the roads were not yet plowed. I was in and out of consciousness the 3 hours it took to get to the ER. I only remember being cold, oh so cold. I kept turning up the heat in the car and my husband had to roll down his window because he and our son were so hot. The roads were dangerous.
By the time we arrived, I was “out of my mind,” thinking and saying things that made no sense, and was taken directly back to a room. My 02 sat via a pulse oximeter (you know the little clips they put on your finger?) was in the low 50’s, my BP was 50/30, my heart rate was 130 and my temperature was 104.5°. I remember little of this, except they’d turned my cot upside down and I was sure I was going to fall out and the giant cockroaches in the ceiling were going to eat me (hallucinations) and I began to vomit and dry heave and didn’t have the strength to turn my head. I’ve been told the story many times with family and discussed with them what I remembered. I was transferred to ICU with several IV’s, oxygen, heart monitor. Blood cultures were taken, chest catheter removed, antibiotics started, and of all times to happen, I started my period. I was completely weakened but remember one of my home training nurses arriving in my ICU room to do a dialysis treatment. I saw her sweet face and just let the dam of emotions release. I cried and cried. All the while, she gave me a sponge bath and helped clean me up. I hurt, I shivered, I cried, she cleaned and dressed me as I received that precious gift of dialysis. It was truly a bittersweet memory.
I settled into a routine of various doctors popping in my room to discuss bloodwork or results of scans and continuing plan of care. Due to the severity I was also meeting respiratory therapist twice daily, physical therapy twice daily, dialysis three times weekly and the dietitian who kept bringing in those little cans of Nepro. I had nausea, vomiting, diarrhea. There were MRI’s, CT scans, ultrasounds, sonograms, trans-esophageal echocardiogram (to rule out infected heart valves), nuclear studies to rule out infections in the bones or lungs or any other body parts. There was also a bone marrow biopsy on the same hip that was so painful for me.
I began having difficulty coping. My husband could only visit once a week. Our youngest son had said goodbye as he left for basic training and our youngest daughter was so frightened by how ill I looked she wouldn’t come to visit anymore. When my husband did visit he would bring little stuffed animals and once brought me in an Arby’s sandwich. He would call me every morning to hear news from the doctors and in the evening to tell me goodnight. I hated being gone from home, stuck there week after week and deteriorating in so many ways. I chose to cope through scans, tests, treatments by counting to myself. I would count to 60 and hold out 1 finger. Once I had counted out 10 minutes, I would start over. I kept telling myself that if I could make it through just one minute then I could keep going. Then if I could manage just 10 minutes, I could keep going. I was emotional when new tests or scans were ordered or when the physical therapist would arrive and want me to sit or practice lifting my legs or try to just walk to the door. I missed home. I missed family. I missed feeling well and a sense of normalcy. For weeks they continued with the IV antibiotics, but the fevers, chills, vomiting, diarrhea and positive blood cultures continued. My platelets dropped, my albumin dropped, my hemoglobin dropped—and then began the hemolysis.
Unfamiliar with the term hemolysis? So was I. Now it’s etched into my brain. According to the Encylopaedia Britannica “Hemolysis is the breakdown or destruction of red blood cells so that the contained oxygen-carrying pigment of the hemoglobin is freed into the surrounding medium.” 2 Sound confusing? Here’s a drawing.
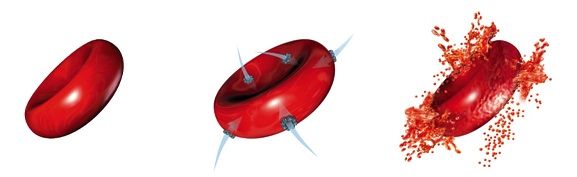 (photo - http://www.secondchanceaihadogs.com/wp-content/gallery/glossary/hemolysis.jpg )
(photo - http://www.secondchanceaihadogs.com/wp-content/gallery/glossary/hemolysis.jpg )
Here is my personal explanation. Let’s say you have a bathtub full of water. You place many balloons in the tub, all filled with red water. Now, imagine the balloons’ structure deteriorating and dissolving in the water so the balloons can no longer hold in the red water. Basically, the balloons disintegrate. This is what happens with the red blood cells in hemolysis. What this meant for me was not enough oxygen rich red blood cells getting to my organs, brain, tissues etc. Low hemoglobin, low platelets. This meant bleeding of my gums, bleeding from my nose, eyes, and ears occasionally, bleeding when urinating, and ginormous blood clots in my uterus and gallbladder.
They thought my gallbladder was so inflamed they took me to surgery to remove it, only to discover a very large (baseball sized) blood clot. Then began the blood transfusions (11 total) and infusions of bags of platelets (7 total). I couldn’t walk, or dress and needed help to wash and sometimes eat. Finally, one day, the infectious disease doctor asked, “Now you have a fistula, right?” Wrong! My nephrologist knew, the nurses knew, and I thought he knew that I had a graft. I could see the “aha” light go on in his head. Back down to nuclear medicine: the graft lit up like a Christmas tree. The graft was infected. Every dialysis treatment when they inserted those needles, it just stirred up the infection. I would shiver, vomit, bleed, and more. The graft was removed, the fevers stopped, shivering stopped, hemolysis stopped, pained lessened. Approximately 4 days after graft removal and 10 weeks after admission I was finally released from hospital. The long rough road of recovery lay ahead.
Why Should My Experience Matter to You?
If you are over 65, diabetic, on dialysis, have chronic kidney disease, have a transplant, have lung issues or any other type of chronic illness, then what you’ve read about my first sepsis experience could just as easily happen to you. Or, worse! When I said 30% of those with sepsis don’t make it, that means 3-4 out of 10 people who get sepsis never come home. Think about 10 of your friends who’ve had a transplant or are on dialysis. Now imagine 3 of them having funerals. It’s not a pretty picture. Don’t want to think about it? I get it. The difficult part is even when we take all the precautionary prevention sepsis can still happen.
Protect yourself and your loved ones from sepsis through prevention. When training for home hemodialysis, we were taught to wash our hands in hot water for 90 seconds—about how long it takes to sing “Twinkle Twinkle Little Star” four times—before rinsing. Some have been taught that 15-30 seconds is enough. Just be sure to wash your hands well and often when you deal with any type of wound or opening through the skin. Our skin is our greatest infection prevention. It is our largest organ and does a great job of protecting us from injury or illness. We should do what we can to help:
Keep skin from getting too dry, so it doesn’t crack.
Avoid cuts and sores on feet, and inspect them daily with a mirror or have someone else check them daily, especially if you are over 65 or have diabetes.
Keep wounds clean and dry and covered from dirt and bacteria.
If you have any cuts, blisters, wounds watch for redness and swelling.
If these signs are present or worsen contact your doctor right away.
The CDC, Sepsis Alliance, and other groups give these tips to prevent or manage sepsis: 3
Prevent infections. Self-manage well any chronic conditions you may have like diabetes, high blood pressure, lung issues, etc.
Stay up to date on any necessary vaccines.
Practice good hygiene. Wash your hands (sing while you wash). Keep cuts clean and covered until healed.
Know the signs and symptoms of sepsis.
ACT QUICKLY. If you suspect sepsis or have symptoms of an infection that isn’t getting better or is getting worse seek medical care right away.
How to Prevent Sepsis on Dialysis
Sepsis is the second leading cause of death in hemodialysis patients. Besides the other tips that are for everyone:
- Check your vascular access daily. If you notice any signs of infection such as redness, puffiness, pus or swelling talk to your healthcare team right away.
- If you have a catheter, keep it covered and dry. If it gets wet, have your clinic nurse replace it with a clean dry bandage.
- Be sure healthcare professionals wash their hands and put on fresh gloves before and after they touch your access.
To Learn More About Sepsis
From the Sepsis Alliance:
Sepsis risk factors: https://www.sepsis.org/sepsis/risk-factors/
Prevention: https://www.sepsis.org/sepsis-and/prevention/
Symptoms: https://www.sepsis.org/sepsis/symptoms/
From the Centers for Disease Control and Prevention (CDC)
A fact sheet: https://www.cdc.gov/sepsis/pdfs/Consumer_brochure_its-time-to-talk-about-sepsis-P.pdf
Sepsis symptoms and diagnosis: https://www.cdc.gov/sepsis/diagnosis/index.html
References


Comments
Taisohn wofford
Jan 11, 2020 8:32 PM
Gale Schulke, RN
Sep 25, 2018 4:15 PM
Many sepsis patients end up on a ventilator, intubated.
As a result of my own experience with Sepsis, I am very aware of the symptoms and get my patients to the hospital quickly when they are starting to develop symptoms.
I am forwarding your article to all of my staff, by the way.