What the Advancing American Kidney Health Initiative (AAKHI) Executive Order May Mean for You

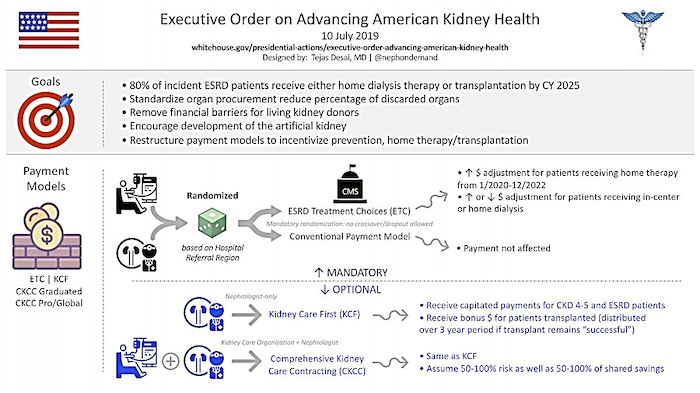
On July 10, 2019, President Trump signed an Executive Order (EO)1 that may lead to changes for patients and dialysis clinics and nephrologists. The EO expressed concerns about the large number of people who progress to kidney failure, which is costly and can adversely affect patients’ quality of life. The stated goal of the EO is to reduce the number of people who progress to kidney failure by 25% and to treat 80% of those who do have kidney failure with transplants or home dialysis. There is one mandatory and four optional models to achieve these goals.
ESRD Treatment Choices (ETC) Model2
Under the proposed mandatory ETC Model, “Managing Clinicians” and dialysis clinics in certain geographic areas of all 50 states and D.C. that treat 50% of adult Medicare patients would be randomly selected to participate. “Managing clinicians” are physicians and other practitioners who treat dialysis patients and bill Medicare for a monthly capitation payment. Dialysis clinics would be excluded if they are in U.S. Territories or treat too few patients or pediatric patients.
What Patients Are Credited and Which Ones Are Not
Patients would be excluded from the ETC model if they are living outside the U.S., are under 18, in hospice, have dementia, or are on dialysis due to acute kidney injury. A risk adjustment would be made for clinics that treat sicker—or healthier—patients. Patients would only be credited to a dialysis clinic or managing clinician if they have Part B. In addition to the exclusions above, patients in Medicare Advantage or other Medicare managed care plans would be excluded. CMS will use Medicare claims and administrative data to determine the risk-adjusted home dialysis rate. CMS will use Medicare claims, administrative data and data from the Scientific Registry for Transplant Recipients (SRTR) database to determine the risk-adjusted kidney and kidney-pancreas transplant rate. Dialysis clinics and Managing Clinicians would be credited for patients receiving kidney or kidney-pancreas transplants, but only Managing Clinicians would be credited for patients receiving pre-emptive transplants.
Patient Protections
Patients will not be able to opt out of the ETC payment model if they are at a selected clinic—but they will be able to choose whether or not to get dialysis from a provider under the ETC Model, and there would be no change in their cost sharing either way. Dialysis clinics and Managing Clinicians would have to post a sign saying that they are taking part in the ETC Model. Because there are incentives in the model that might affect practices, CMS will monitor for “steering, coercion and in appropriate referrals” using claims data, reviewing medical records, and surveying and interviewing patients.
Payment Adjustments
The model proposes two payment adjustments:
Payments to clinics and Managing Clinicians who treat home dialysis patients would be higher for the first 3 years.
Payments would be adjusted over time depending on how well or poorly a clinic or Managing Clinician performs in improving home dialysis or transplant rates.
According to the proposed regulation3, a home dialysis payment adjustment (HDPA) for dialysis clinics would be added to the payment dialysis clinics get under the ESRD prospective payment system (ESRD “bundle”) and to clinicians’ monthly capitation payment, at a schedule of:
+3% in 2020
+2% in 2021
+1% in 2022
Dialysis clinics and managing clinicians would be awarded a modality performance score (MPS) for patients on home dialysis and who receive transplants. This score is based on the higher of the achievement or improvement score, with 2/3 of the score for home dialysis and 1/3 for transplant.
Here is how CMS proposes to calculate the achievement score:
90th+ percentile of benchmark rates for comparison geographic areas during the benchmark year: 2 points
75th+ percentile of benchmark rates for comparison geographic areas during the benchmark year: 1.5 points
50th+ percentile of benchmark rates for comparison geographic areas during the benchmark year: 1 point
30th+ percentile of benchmark rates for comparison geographic areas during the benchmark year: 0.5 points
<30th percentile of benchmark rates for comparison geographic areas during the benchmark year: 0 points
Here’s how CMS proposes to calculate the improvement score:
Greater than 10 percent improvement relative to the benchmark year rate: 1.5 points
Greater than 5% improvement relative to the benchmark year rate: 1 point
Greater than 0% improvement relative to the benchmark year rate: 0.5 points
Less than or equal to the benchmark year rate: 0 points
Effective Dates
As proposed, the home dialysis and transplant rate measurement years would be January 1, 2020 through June 30, 2025 (may start and end 3 months later). The performance payment adjustment (PPA) period to ETC participants would be from July 1, 2021 through June 30, 2026. CMS projects that by 2026, 19% of all Medicare patients on dialysis in selected geographic areas will be dialyzing at home.
Evaluation
CMS plans to evaluate the effectiveness of the model by comparing managing clinicians and dialysis clinics participating in the model with those in regions that are outside of the model. Clinics would be matched on home dialysis and transplant rates, Medicare spending before the model, patients’ sociodemographic and clinical characteristics, and other factors. CMS will assess the impact of this initiative on deaths and hospitalizations.
Kidney Disease Education
Previously only physicians, nurse practitioners, clinical nurse specialists and physician assistants were considered “qualified providers” for Medicare’s Kidney Disease Education (KDE) benefit. The ETC Model would allow others including nurses, dietitians, and social workers to provide KDE to patients under a Medicare-enrolled participating Managing Clinician. It also allows KDE to be provided by telehealth. Previously the only Medicare patients eligible for KDE were those with Stage 4 CKD. The proposed regulation would expand access to Medicare patients with Stage 5 CKD. It would also expand KDE to Medicare ESRD patients during the first 6 months after their ESRD diagnosis. The regulation also proposes to waive the Part B copay. The goal with these changes is to increase the percentage of Medicare patients who get KDE services from around 2% to 3.2% by 2026.
Transplantation
Although the Administration hopes that more people will get transplants, which can save Medicare money, this proposed regulation did not set a goal for increasing the number of transplants. It notes that education could decrease the discard rate from 19% to 15%. Education and incentives to dialysis clinics and Managing Clinicians may cause the size of the deceased donor transplant list to grow. However, investing in patient education may help more patients find living donors, especially if financial disincentives can be reduced. The ETC Model doesn’t propose additional funding for the National Living Donor Assistance Program. This program provides up to $6,000 for certain expenses for living donors if a donor and recipient’s income is below 300% of federal poverty. The proposed regulation stated that in 2017 only 8.38% of living donors got this help.
Questions About the ETC Model
Will clinics in the ETC model be selected from those already Medicare certified to offer home dialysis training and support? At this time of the 7,564 Medicare-certified dialysis clinics in the U.S., 1,621 (21.4%) are certified to provide home hemodialysis training and support, 3,299 (42.6%) are certified to provide peritoneal training and support, and 28 (0.4%) are certified for home training and support only. 4 If dialysis clinics are selected that are not certified to offer home dialysis training and support, this could require time and investment in infrastructure including designating at least one room for home training, hiring a registered nurse who meets the ESRD Conditions for Coverage personnel qualifications at 42 CFR 494.140(b)(2), establishing contracts with suppliers of home dialysis equipment and supplies, recruiting and training at least one home patient, requesting a survey, and being certified for one or both home dialysis options. If patient recruitment is slow, a home training nurse may have to cover multiple clinics, work in the in-center area as well as home training, and lack of experience in troubleshooting patient problems could adversely affect clinic outcomes in the ETC model and increase patient depression.
Optional Models
CMS is also proposing optional models that would provide incentives to nephrology practices or groups of healthcare providers to manage kidney disease better along the continuum from CKD to dialysis and/or transplant. Requests for applications are intended to be published in August 2019. These proposed models would run from January 1, 2020 through December 31, 2023 with the option to extend for 2 more performance years:
Kidney Care First (KFC)
Comprehensive Kidney Care Contracting (CKCC)
Graduated CKCC Professional
CKCC Global.5
Under the Kidney Care First Model, nephrologists and their practices would get a capitated payment based on CKD Stage 4 and 5 patients’ health outcomes, experience, and other standards. They would also get a bonus payment for transplants that would be paid over 3 years post-transplant, as long as the transplant is still successful.
The three different Comprehensive Kidney Care Contracting Models are required to include nephrologists and transplant providers. They would follow different approaches. All are proposed to improve patient management with different levels of risks and rewards.
Here’s an infographic from the American Society of Nephrology that attempts to explain this complex proposed regulation simply.6
Public Comment
The regulation is now published at https://www.regulations.gov/document?D=CMS-2019-0101-0001. Click on the PDF icon beside “View original printed format” to read the 118 page proposed regulation. Part is about radiation oncology and part is about kidney disease. Only the last 7 pages (34589-34595) describe the proposed regulation. The rest of the text explains the proposed regulation. Click the "Comment Now" button to make your comment online. Information on how to comment by mail or fax is in the PDF. No matter how you comment, be sure to say you’re commenting on CMS-5527-P. The comment period closes on September 16, 2019 at 11:59 p.m. All comments are posted for public viewing so keep that in mind when making a comment. There is a link to “Open docket folder” that will take you to a page where you can read comments. Be aware that some will be about radiation oncology. If you like, dislike, or have suggestions, please comment. That's the only way your voice can be heard. These are just a few of the topic areas where the proposed regulation is seeking comments.
Whether participation in the ETC Model should be mandatory
Where dialysis clinics are located for selection for the ETC Model
Where Managing Clinicians are located for the ETC Model
Whether the HDPA should be applied to Medicare secondary payer claims for dialysis clinics and Managing Clinicians
Whether current adjustments to the ESRD PPS should be excluded by the HDPA
What Condition codes to use to identify home dialysis (proposes 74, 75, 76, and 80)
Whether the patient cost-sharing would not be affected by the HDPA
Whether the transplant rate should be included in the modality performance score
The schedule for measurement year and performance payment adjustment period
Proposed beneficiary exclusions and whether patients over a certain age should be excluded from being counted for a participating ETC clinic/Managing Clinician
What data to use to determine home dialysis and transplant rate
Methodology to assess home dialysis rate for ETC participants
Changes in Kidney Disease Education benefit
Beneficiary protections
Monitoring of unintended consequences and equipment problems
Quality measures (Standardized Hospitalization Rate and Standardized Mortality Rate)
Evaluation of the proposed ETC Model
Learn More About Chronic Kidney Disease and Home Dialysis with Evidence-based Resources from MEI:
Staying Healthy with Stages 1-3 CKD.
Living the Life You Want with Stage 4 & 5 CKD
How to Have a Good Future with Kidney Disease FREE CKD education slides
Implementing Hemodialysis in the Home
Home Dialysis Central - https://homedialysis.org/
-
Conclusion
This initiative is an ambitious one and only time will tell how well it will meet its goals. Medical Education Institute has devoted decades to educating patients and professionals and advocating for patients’ improved access to and utilization of home dialysis. Many patients want and need to be in greater control of their health and lives. Opening more doors to home dialysis will allow them to assume that control.

Trump DJ. Executive Order on Advancing American Kidney Health. https://www.whitehouse.gov/presidential-actions/executive-order-advancing-american-kidney-health/ (Accessed 7/14/2019)↩
Centers for Medicare & Medicaid Services Newsroom. Proposed End-Stage Renal Disease Treatment Choices (ETC) Mandatory Model. June 10, 2019. https://www.cms.gov/newsroom/fact-sheets/proposed-end-stage-renal-disease-treatment-choices-etc-mandatory-model (Accessed 7/14/2019)↩
Centers for Medicare & Medicaid Services. Medicare Program; Specialty Care Models to Improve Quality of Care and Reduce Expenditures. 42 CFR Part 512. https://www.hhs.gov/sites/default/files/CMS-5527-P.pdf↩
Centers for Medicare & Medicaid Services. Quality, Certification, and Oversight Reports. Dialysis Facilities (ESRDs). https://qcor.cms.gov/main.jsp (Accessed 7/15/2019)↩
Centers for Medicare & Medicaid Services Newsroom. Kidney Care First (KCF) and Comprehensive Kidney Care Contracting (CKCC) Models. June 10, 2019. https://www.cms.gov/newsroom/fact-sheets/kidney-care-first-kcf-and-comprehensive-kidney-care-contracting-ckcc-models (Accessed 7/14/2019)↩
American Society of Nephrology. KidneyNews Online. https://www.kidneynews.org/careers/resources/infographic-new-payment-models-proposed-by-advancing-american-kidney-health-executive-order (Accessed 7/16/2019)↩


Comments
Nancy Verdin
Jul 26, 2019 4:59 PM
1. For people renting: unless their land lord approves, in writing (at least in Alberta, Canada) then the necessary renovations to accommodate the dialysis machine, most property owners fear the potential for water damage so much they won't allow it).
2. Home hemo is not free for the patient, there are additional power and water costs associated with it that is not automatically covered by any service that I know of.
3. Some home dialysis programs require the presence of another person "just in case .." for many who live solo this is not an option .. also in some cases it must be a family member which eliminates another large group of patients.
On another direction when it comes to transplantation the cost of the meds alone eliminate many people ... and lastly those who are not eligible due co-morbiditys and conditions like antibody mediated rejection so transplant is also out the question.
I don't see where any of these areas are addressed in the new EO ... I see mostly $ signs in the EO .. nothing about people at all or the complexity of kidney failure and treatment.
Eric Weinhandl
Jul 24, 2019 11:56 PM
In 45 patient-years, the average number of transplants in persons between ages 18 and 75 years is somewhere between 1 and 2. This really complicates facility-level assessment of achievement and/or improvement. We have a "small numbers" problem, despite the best of intentions.
Beth Witten
Jul 25, 2019 3:34 PM
Eric Weinhandl
Jul 25, 2019 10:31 PM
Raymond Aguilar
Jul 24, 2019 4:21 PM
Beth Witten
Jul 24, 2019 5:01 PM
Beth Witten
Jul 24, 2019 4:14 PM
Dori schatell
Jul 24, 2019 1:15 PM
Corry Walker
Jul 24, 2019 12:06 PM
John Agar
Jul 23, 2019 9:35 PM
Excellent and useful blog, though not being ‘in’ the US system and not having to negotiate and understand this stuff, I am actually not well placed to comment on the detail.
The stand-out thing that bothers me about Trump’s Executive Order is the potential for huge unintended consequences.
Home dialysis can only succeed if two ‘unmentioned’ and, I fear, ‘poorly recognised’ factors that seem to be missing from this rush-of-blood EO
1. A careful specialty-wide education process … not of the patient going home, or (peculiar to the US) of a care-giver … but of the professional staff [nurses and doctors] who administer, oversee, advise, support, and empathise with their home patients.
2. An in-depth core understanding of the principles of dialysis - both PD and HD - and how the various ‘levels’ that allow any one individual’s dialysis program to be elevated from subsistence care (NB: the euphemism ‘adequate’ is sometimes used as a substitute for subsistence), to an achieved optimum, best-in-class outcome.
I may be behind the times with my data now - though, somehow, I don’t quite think I am - but it was only 5 years ago that data was presented by Bob Lockridge (an unchallengeable US home HD guru from Lynchburg, WV) and Dori Schatell (from Home Dialysis Central and the Medical Education Institute in Madison WI) that noted:
1. Less than 10% or US Fellow training programs actually trained for or exposed training Fellows to home dialysis [Bob Lockridge]
2. Only 3/100 questions on the Nephrology Boards Examination were about dialysis, dialysis principles, or dialysis management - let alone home dialysis … on which there were none! [Dori Schatell]
Unless I am sadly mistaken, this lack in training, in exposure, in education, and in experience has not materially changed since that data was presented.
Throwing Executive Orders and Federal money at home dialysis without the basic groundwork in training and experience to advise, oversee, and manage dialysis at home risks seeing a financially incentivised rush to push patients into the home, but without a matching expertise to manage them there.
This may result in appalling home outcomes for a great many unsuspecting patients.
Home dialysis is not just about saving money - though I fear this is the subtext of Trump’s EO - but should be about patient empowerment, patient self-autonomy, and patient outcomes.
Unless urgent attention and synchronous attention is given to nephrology training programs - both physician and nurse - then I fear these latter and laudable goals may be submerged in a sea of poorly trained and executed programs - to the long-term detriment of home care. Further, good training requires an experiential base to build from ... and that base is sadly lacking. This suggests the incentivising effort may be dissipated into inertia, with 'savings' and not 'patient benefit' as the key outcome measure.
It would have been more far-reaching if the EO had more sharply examined the reimbursement system and had considered the superb game-changer proposed by Mel Hodge in these blog pages: https://www.homedialysis.org/news-and-research/blog/153-kidney-caucus-letter-repayment-basis . Sadly, it did not.
It will be interesting to see how the dialysis companies work this new EO to their financial benefit - for as sure as eggs they will - and whether the patient again gets lost in the scramble for profit and 'the bottom line'.