Potential Allergic Contributors to Dialysis Symptoms

The overwhelming majority of symptoms associated with dialysis relate to a poorly devised treatment prescription; in particular, an all-too-rapid ultrafiltration rate (UFR, measured in ml of fluid removed per kilogram of patient body weight per hour of dialysis). In turn, the UFR is directly related to the session time prescribed for each treatment. A too-short dialysis session—coupled with excessive interdialytic fluid gain—enforces a high UFR that depletes intravascular volume and leads to a rapid fall in blood pressure, circulatory instability, nausea, vomiting, headache, dizziness, chest tightness and angina in susceptible individuals, and loss of consciousness. In Australia, we call this “going flat.”

However, a small fraction of dialysis-related symptoms may relate to other allergic, inflammatory, or reactive factors that can be generated by dialysis equipment itself. A recent question asked at the Home Dialysis Facebook page can be paraphrased as follows:
“I feel very itchy/fidgety at the end of dialysis. Diphenhydramine (Benadryl ®) helps. I am not itchy on days I don’t do dialysis.”
The inference of the question was whether something related to the dialysis was leading to the symptoms. My answer was, “While it is very rare for dialysis to cause allergic-like symptoms nowadays, it is possible.” So, if the dialysis could be responsible, how or why could that be so?
1. Firstly, there is the dialysis fluid (dialysate) itself, which is made up from:
Highly filtered, purified water. The AAMI and European Best Practice quality requirements that proscibe for ultrapure water in dialysis systems are very stringent. If the filters and RO membranes are appropriately maintained, pre-filtration + reverse osmosis treatment of mains/bore/well/tank water should prevent any water-borne inflammatory substances or endotoxins from reaching the dialyser membrane. Obviously, the operative word here is “should.” To ensure that “should” actually “does,” regular water-quality checks—in particular for endotoxin and bacterial culture—are mandatory.
Powdered or fluid concentrates of electrolytes; predominantly sodium, calcium, potassium, chloride, magnesium, and glucose. These should be accurate, by factory specifications, and should be pure mixtures of only these substances. To be otherwise would indicate a serious breach of manufacturing regulations
A buffer. This is bicarbonate, lactate, or acetate, with bicarbonate clearly the favoured option. Again, the same regulatory specificity is required by law.

For any of these to be out-of-sync would indicate a filtration or factory failure. Of the three, only a failure of water quality would be likely to stimulate any form of “allergic” response, especially if there were to be an endotoxin exposure. Test kits now allow water systems to be regularly verified and ensured “clear” of endotoxic exposure. For the NxStage System One, bagged dialysis fluid may also be used. My comments on this can be taken in combination with my remarks about the plastic consumables (below).
2. Secondly, there is the fluid delivery system: the means by which dialysis fluid is transported from the filtration systems to the dialyser. This pathway is commonly grouped by the term “consumables”—the bits that are thrown away after each treatment. These comprise a complex tangle of plastic tubes and air-traps etc. that both blood and dialysis fluid pathways are exposed to in the extracorporeal (out-of-body) circuits that are loaded onto the dialysis machine. Or, in the case of the NxStage and the Quanta SC+ systems, consumables form part of their pre-formed dialysis cartridges. I will return to this important component shortly.

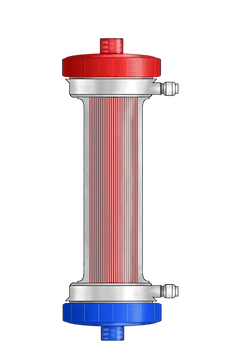
3. Thirdly, there is the dialyser, especially the composition of the membrane. The biocompatibility of membranes has significantly changed and markedly improved since the early cuprophane membrane days. Indeed, my own report of complement activation, pulmonary white cell sequestration, and cardiopulmonary decompensation from cuprophane membranes1 was one of the early signals that membranes could induce an overwhelming inflammatory storm. This is not the place to detail the progress of membrane compatibility, but membranes did (and can still) play a role in dialysis symptoms.
4. Finally, there are additives: purposefully prescribed or accidentally infused IV medication, drug, or supplement additions to the dialysis system. Most common of these are unfractionated sodium heparin (in the US), or low molecular weight heparin enoxaparin (as is used in ANZ). However, there may be a raft of other IV anticoagulant options in use here and there, plus various options in IV iron (in Australia, we use IV ferric carboxymaltose = Ferrinject), erythropoietin in its various commercial forms, a potential range of IV antibiotics that may be required/used from time to time, citrate (or like substances) with or without antibiotics (like gentamicin) where these are used for infection-protective catheter locks, and catheter un-blocking agents like TPA (Alteplase), to name a incompletely inclusive list.
An allergic response to any of these is possible, with unfractionated heparin (perhaps most pertinent to our questioner) known to cause itch as one of its many potential—though blessedly rare—clinical side-effects. If heparin is suspected, a review of inflammatory markers, like an eosinophil count, an erythrocyte sedimentation rate (ESR), a C-reactive protein (CRP), and/or a light chain analysis) may be useful, and, if there is any suspicion of allergy, a change to low molecular weight heparin may be an option.
But consumable plastics are the potentially most interesting of the four. This area remains the most contentious. Plasticisers have long been known to be potential toxins and/or inflammatory stimulators and have always been a potential source of dialysate contamination. There are a raft of suspect plastic metabolites: di(2-ethylhexyl)phthalate (DEHP), mono(2-ethylhexyl)phthalate (MEHP), 2-ethylhexanol (2-EH), and phthalic acid (PA), while a significant further suspect contributor to human illness are the cyclohexanones—substances used in the glues that bind plastic tubing(s) together.

DEHP has been assessed in an in-depth FDA report with one study within that report [Faouzi et al] suggesting that ...
“On average, 75.2 mg of DEHP was extracted during a single dialysis session, with a range of 44.3 to 197.1 mg. However, while not all infused DEHP an estimated 3.6 to 59.6 mg of DEHP is retained in a single dialysis session. Assuming 3 dialysis sessions/ week, this dose is equivalent to a time-averaged dose of 0.02 to 0.36 mg/kg/day for a 70 kg patient.”
https://www.fda.gov//images/blog/1-30-20/114001/download
Cyclohexanone is a bit of a nasty piece of work. Not only has it been implicated in human symptomatology, but it is the glue primary used to connect and/or bond most commonly used IV, extracorporeal [and dialysis tubing] sets together.2 Several studies have confirmed the presence of cyclohexanone in the dialysis extracorporeal dialysis circuit, one such being found at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716145/
One issue that has not yet been investigated—at least to my knowledge—is the effect of transport on the plastics, fluids, and equipment used in dialysis or, to for that matter, in any healthcare situation. Fluids and plastics are often transported by truck over long distances, during which they may be exposed to extremes of hot or cold weather. The effects of this and other potential environmental influences may prove crucial to product(s) later delivered to and used in good faith by both incentre services or home patients. Might sunlight, heat or cold “trigger” generation and/or release of harmful metabolites from the plastics we later use so innocently in the extracorporeal circuit? To be frank, I doubt we truly know.

Unfortunately, there are as yet no other practical options in the delivery of dialysis other than to use plastics. Luckily and as best we know it, the clinical sequelae from their use are minimal—or at least it appears that way for the vast majority. But plasticisers and plastic bonding agents remain a potential Achilles heel in the purity of the dialysis process.
We should study more…know more…admit more… and demand more information from companies/industry than we currently have, or receive, about the potential and actual toxicity of the equipment, fluids, and systems we are required to use.
As all “environments”—whether macro or micro—are finally assuming a rightful importance in our 21st century, the microenvironment(s) we provide for both dialysis fluid and blood must also draw far greater attention. Plastic is not an inert non-contributor to the dialysis milieu but is likely a key component that may/can interact with its passenger fluids. Our exploration of this interface and interaction remains rudimentary. Can plastics, plasticisers, and glue be harmful? Be allergenic? To be honest, it is time we knew more.
Agar JW, Hull JD, Kaplan M, Pletka PG: Acute cardiopulmonary decompensation and complement activation during hemodialysis. Ann Int Med. 1979 May;90(5): 972-973↩


Comments
Sally Diavatis
Jul 13, 2023 9:01 PM