The End Stage Renal Disease Treatment Choices Model Includes In-center Self Care

On July 10, 2019 President Donald Trump signed the Executive Order on Advancing American Kidney Health, which directed the Department of Health & Human Services to develop a reimbursement model to incentivize use of home dialysis and transplant. The 268-page final rule, Medicare Program; Specialty Care Models To Improve Quality of Care and Reduce Expenditures, including regulations for the End Stage Renal Disease Treatment Choices (ETC) Model, was published in the Federal Register on September 29, 2020.

The “preamble” or list of community comments and CMS responses is from page 61114 to page 61374. In the PDF, the regulation text for the ETC Model is only 8 pages long, from 61374 to 61381. The ETC Model addresses reimbursement changes related to home dialysis and transplant for dialysis facilities and Managing Clinicians who treat patients with traditional Medicare, not those with Medicare Advantage plans. This blog will focus only on in-center self-dialysis in the ETC Model. If you search for “self-dialysis” in the regulation text, you will find it 39 times, mostly related to the training add-on for home and self-dialysis modalities.
Background
For the ETC Model, CMS will select dialysis facilities that serve 30% of adult Medicare patients from a random sample of geographic areas called “hospital referral regions” (Excel in zip file). Those clinics and patients will be required to participate. Clinics will report data on home dialysis and transplant rates during the measurement years from January 1, 2021 through June 30, 2026. The clinics that show outcome improvements will receive higher reimbursement under the performance period adjustment (PPA) from January 1, 2022 through June 30, 2027. 
Comments to the proposed regulation suggested providing credit for in-center self-care. CMS agreed that on 072X type claims during each measurement year (MY), it will count traditional Medicare patients in the Model this way:
-
Full credit for patient months with condition code 74 or 76 (home dialysis), plus
-
Half credit for patient months with condition code 72 (in-center self-care).
While we don’t know what will happen, this payment strategy raises some intriguing questions.
-
Will the incentive to count in-center self-care in the ETC Model encourage more clinics to start self-care programs?
-
If more clinics offer in-center self-care, will patients see others doing their own dialysis and test their own ability to run their dialysis?
-
Will more clinics encourage patients who have proven they can do in-center self-care to do home dialysis—with or without a care partner?
In-center Self-care Defined
CMS has expectations for in-center self-care. the Medicare Benefit Policy Manual (ESRD), Chapter 11 provides this definition in Section 10: “Self-Dialysis - Dialysis performed by an ESRD patient in-facility with the expectation that the patient performs their dialysis treatment with little or no professional assistance. The patient must have completed an appropriate course of training as specified at 42 CFR §494.100(a).” An added note states: “Self-dialysis and home dialysis include training programs that educate ESRD patients and/or other individuals to assist the patient in performing self-dialysis or home dialysis with little or no professional assistance.”
Why a Clinic Might Choose to Offer In-center Self-care
Here are some possible reasons:
-
Dialysis clinics that are certified to provide home HD training can bill and be reimbursed by Medicare for training Medicare patients to do in-center self-care as long as the training is the same as for patients/care partners who do dialysis at home, including meeting the requirements at 42 CFR 494.100(a):
Be provided by a dialysis facility that is approved to provide home dialysis services;
Be conducted by a registered nurse who meets the requirements of § 494.140(b)(2);
Be conducted for each home dialysispatient and address the specific needs of the patient, in the following areas:
(i) The nature and management of ESRD.
(ii) The full range of techniques associated with the treatment modality selected, including effective use of dialysis supplies and equipment in achieving and delivering the physician's prescription of Kt/V or URR, and effective administration of erythropoiesis-stimulating agent(s) (if prescribed) to achieve and maintain a target level hemoglobin or hematocrit as written in patient's plan of care.

(iii) How to detect, report, and manage potential dialysis complications, including water treatment problems.
(iv) Availability of support resources and how to access and use resources.
(v) How to self-monitor health status and record and report health status information.
(vi) How to handle medical and non-medical emergencies.
(vii) Infection control precautions.
(viii) Proper waste storage and disposal procedures.
-
Dialysis clinics may have a higher return on investment when offering evening or nocturnal shifts for patients willing to do in-center self-care who are working. Labor costs for those shifts may be less than for full-care shifts with higher patient-to-staff ratios and revenues may be higher when patients have employer group health plans.
-
In-center self-care patients may feel and do better, in terms of higher self-confidence, self-esteem, and improved outcomes.
-
Staff may have higher job satisfaction when working with in-center self-care patients who are more engaged and less dependent on them. This may reduce costly staff turnover.
Numbers of Clinics that Currently Offer In-center Self-care
It is hard to tell how many clinics will make this option available to patients. The CMS 2728 Field 40 asks whether self-dialysistraining is for HD, CAPD, CCPD, or Other and whether training is for home or in-center. CROWNWeb, administered by the Health Services Advisory Group (HSAG), tracks these data. The United States Renal Data System gets data from CROWNWeb and reports prevalence data for modalities, including in-center self-care. According to Table D.11 (opens in Excel) from the 2019 United States Renal Data System Annual Report,1 in 2017 (the most recent data) there were 522 patients doing in-center self-care in the U.S. Dialysis clinics do not need separate certification to offer in-center self-care, so Dialysis Facility Compare does not include an option to locate a clinic that offers it. HSAG or researchers with the USRDS may know where these patients are doing dialysis.
Outcomes for In-center Self-care
More research is needed, but in one study2 that compared in-center self-care patients and matched controls on traditional in-center HD for a 3-year period, researchers found that the self-care patients had:
-
Fewer hospitalizations per patient year (0.02 to .07; p <.05)
-
Fewer deaths per patient year (0.82 to 1.70; p <0.008)
-
Fewer missed treatments when looking at all treatments (1.1% to 3.8%; p < 0.005)

Encouraging Progress Toward Self-care
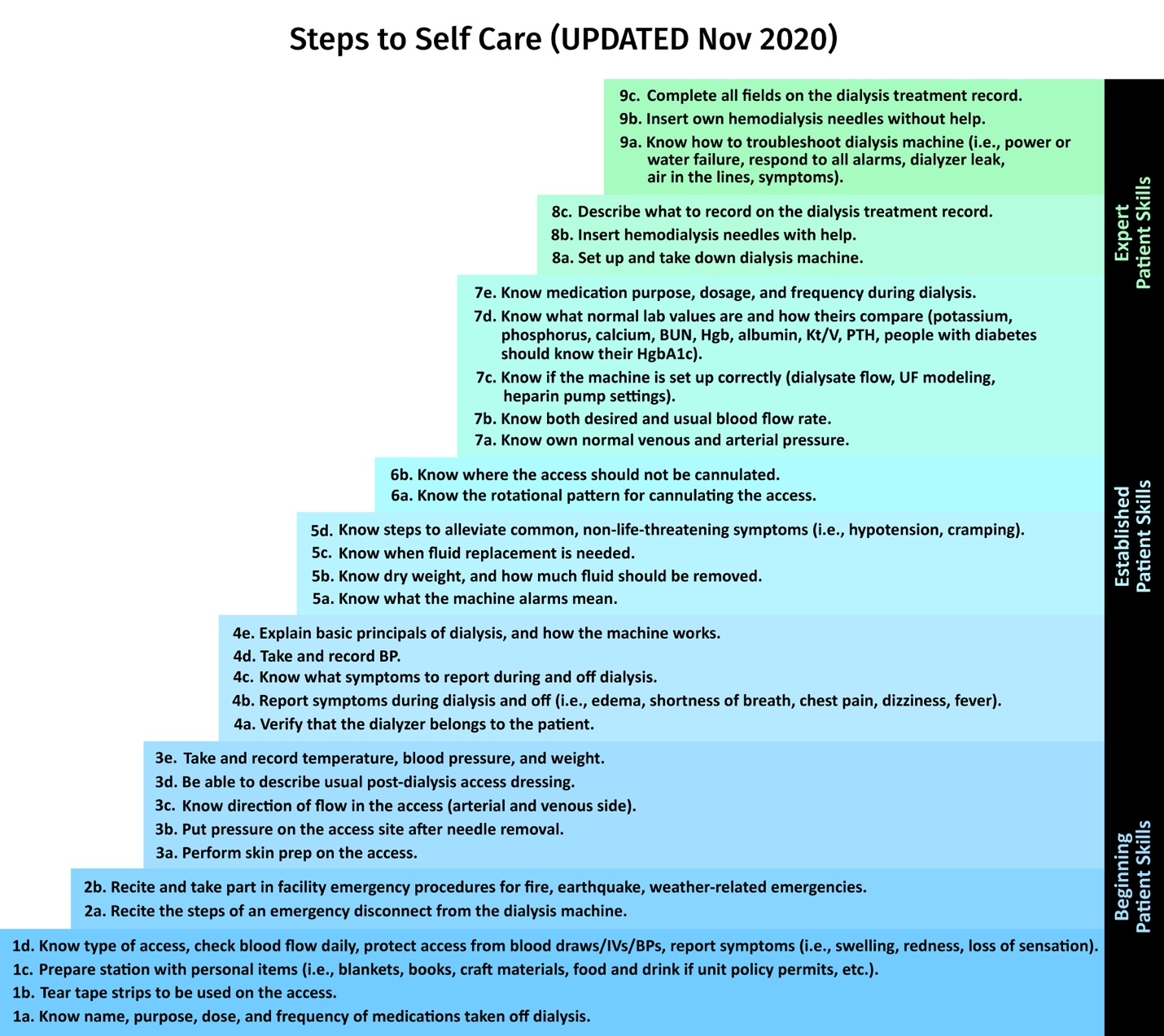
Even if a clinic is not certified to provide home HD training, staff can provide education and reinforce an expectation that patients who are capable should be encouraged to participate as fully as they desire in their care. Participation in care is a patient right mandated at 42 CFR 494.70(a)(5). Although it may take staff time to teach patients to do self-care steps, the time saved in the long run could be significant—while reducing the stress on staff and patients who in a typically fast-paced dialysis clinic feel like they’re on a hamster wheel or assembly line. To help staff know what these steps include, Medical Education Institute’s Building Quality of Life: A Practical Guide to Renal Rehabilitation provides this graphic, which is numbered to read from the bottom to the top.
Conclusion
In-center self-care is an underutilized treatment option for patients on dialysis. Patients may not be aware that they could do self-care, and staff may not know that in some cases training can be reimbursed. The new ETC Model may open more eyes to this treatment option that was common in the early days of dialysis. Even if patients today are older with more comorbidities, they should be evaluated as a candidate for self-care in-center or at home.
For more information
-
CMS, End-Stage Renal Disease Treatment Choices (ETC) Model Fact Sheet
-
Medical Education Institute, Inc., In-center Self-Care: New Interest in an Old Idea in In Control (September 2007)
-
American Association of Kidney Patients, Increasing Self-Care Dialysis Adoption (March 2008)
-
Kidney News Online, In-center Self-care Hemodialysis: An Idea Whose Time Has Come? (March 2017)
1United States Renal Data System. 2019 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2019. https://www.usrds.org/annual-data-report/
2Jones ER, James L, Rosen S, Mooney A, Lacson E Jr. Outcomes among patients receiving in-center, self-care hemodialysis. Nephrol News Issues. 2016 Sep;30(10):28, 30-6. PMID: 30512279. https://pubmed.ncbi.nlm.nih.gov/30512279/


Comments
Beth Witten
Mar 15, 2021 6:50 PM
Jeanne Beck
Mar 12, 2021 4:42 PM