Care Partner? Me? A “Dialysis Tech at Home” for My Loved One? NO WAY!

Hi there, my name is Michael Howington and if you are reading this, you may be in the same boat, (possibly with the same or higher levels of anxiety) that I was recently. You may be overwhelmed with your loved one’s health, dialysis, treatments, and the like. You may be thinking, “There’s no way I or we can do this at home, there is too much that can go wrong, I am not a nurse or a dialysis technician.”
This post attempts to guide you through your journey, a journey that has good news—others HAVE been in the same place that you are now, and they are thriving. Before I get started, let me give you a brief overview of how I got here.
My wife has a host of medical problems and in 2018, starting with the flu, we were in the hospital at least once a month for various issues. Her CKD (chronic kidney disease) was not newly diagnosed; she was in the end stages of the disease. Her care team at that time had established that dialysis was too risky for her situation (what led to CKD began with renal stenosis on one kidney leading to atrophy.)
The danger for her with dialysis was stroke or heart attack because of blood pressure and circulatory problems. They determined the risk was too great and believe it or not, she had accepted her gradual decline that would eventually lead to her death. Yes, you read that correctly, she had accepted her fate and was content to live as much “life” as she could, following the kidney friendly diet, and taking every precaution to live as long as she could but had accepted that her days were numbered.
Over the course of these years, her health slowly declined, at times with her bi-weekly lab appointments, we obsessively watched her “magic numbers” (you know the ones I mean, creatinine and GFR) and at times her kidney function improved, but it generally stayed within a 19%-28% range until 2018. What was a steady decline then became a rapid one.
In the beginning of fall of 2018, the flu she contracted led to pneumonia, early congestive heart failure, and broken ribs. (I promise, I didn’t do it! She was coughing so much, and her bones and body were so frail she broke two ribs). Her care team at the time essentially gave up and sent her home. We were not sure if she would make it through Christmas, but much to our surprise she did and to New Year’s Eve. 
On January 3rd, our Belgian Malinois rescue, “Fluffy”, woke her up because she had stopped breathing. The fluid buildup around her heart and lungs made her feel like she was drowning, unable to catch her breath, and her body was weakened. The toxins had built up so much that she was not able to mentally process what was happening. This led to an ambulance ride to the nearest hospital (not her usual one) and 20 days as a patient. The doctors tried everything, but the outlook was grim—she had days at best. The nephrologist basically stated that the dialysis may kill her (high risk for a stroke, heart attack, clots), but at her current rate she would die very soon. They took a risk and believe me when I say, that was almost 2 years ago, and she is doing better than she has in many years! As you may know, the first few treatments tend to wipe the patient out and are very rough on the patient. In her case, she did exceptionally well and felt much better!
We were assigned to the nearest DaVita clinic and her three treatments a week schedule became her daily life. DaVita presented the at-home options and we both were overwhelmed. On one side, we were getting used to this lifestyle, adjustments for treatments and the like, and overwhelmed with the process and all the time treatments take. But, on the other hand, we were nervous about any change. How long would dialysis be an option? How long would it work before she ended up like so many of her fellow “chair mates” being taken by ambulance? When will she get diabetes?”
Eventually, we did adjust and were able to explore at-home options and we chose HHD—home hemodialysis. After the clinic carefully evaluated her ability to be a candidate, we were then told it would be a 6-week training program (for both of us). Six weeks? Are you kidding me?!? We both immediately concluded, it must be difficult, complicated, or better suited for those with a medical background. While she had been a firefighter, and I had been a wilderness EMT (both when we much younger, smarter, and had more energy), we were intimidated with even the length of the training and what that must mean.
Training
First and foremost, I have to stress that before you get to the training stage, some very smart and experienced people have directly (with your knowledge) and indirectly (in meetings that include cross-functional expertise-social worker, nurse, clinic technicians, and doctors) have already judged if you would be a candidate. This is not a decision that is taken lightly, so they have concluded that you CAN do it. This means they believe in you, so now it is your turn to believe in you.
Secondly, this training is designed not only to show you the normal steps for a normal treatment for a nice fair weathered day, but it also takes you through the storms. These storms include problems, but also as all good training should do, how to resolve these problems. After all, your loved one’s life is literally at stake and you should be careful in every step as part of this treatment. I mean, you are helping him or her connect to a machine that takes their blood out, filters it, and puts it back in.
DON’T BE INTIMIDATED!
You’ve got this! I promise, the training in some cases may be longer, but I promise you they will not send you home to start your treatments unless you have convinced them that you are competent, confident, and can actually handle both the treatment and challenges that may arise. They believe in you, so I say again, it is now your turn to believe in you!
Now What?
I must say that just because we finished our training, felt somewhat confident in knowing what to expect, having practiced for 6 weeks on the identical equipment, and being inundated with calls and emails with deliveries and orders and such, we were still quite nervous. While it is not a usual part of the training, I insisted on being able to perform every function, because I still had raw memories of my wife at her worst, mentally, and the need for me to “take over” things that she normally did. Your results may vary, but I would urge you to considering learning each aspect, including the scary cannulation, as you never know what you may “need” to have to do at some point.

Understand this first: Your first job is to be his or her support animal! Perhaps you don’t need a vest and collar to designate you as such but you need to be confident, positive, and encourage him or her in their treatments. I can only observe and imagine what treatment is like, but it seems that some days she just does not feel like doing the treatment. She is a compliant patient, watches the diet, fluid intake, and performs her treatment most of the time as prescribed, but there are days it is a struggle for her to do so. This is your first job. Motivate and encourage your patient.
Secondly, ask the training nurse questions, discuss the various aspects with the patient, as every relationship is different, you know what each other’s limitations are.
In our case, we are told that we have a great relationship, and we are an especially a great team. This is because we “know” each other so well, we can read one another, and we talk (arguably not always as often about topics as we should, but we eventually get there). This is not to brag but to say, we already have a great communication system (verbal and non-verbal). We first discussed the logistics: “where will we do the treatments? Where will the equipment be? Where will our supplies go?” This was overwhelming at first (especially those first deliveries!), but over time we naturally adjusted as we got our own routines down. Fortunately, our first treatments at home were under the supervision of our nurse and quite honestly that did help build our confidence.
As a quick side story, I was once a private pilot. I had a great instructor, we first had ground school (book work), then “right seat flying” (co-piloting), and eventually I did more of the work and he flew in the right seat. Then came the big prize—my first solo flight! I, just like you will, had a lot of training and the CFI’s confidence that I was ready. My first solo flight (I am writing this, so spoiler alert, I survived) I “suddenly starting hearing sounds I had never heard before” during flight. In reality, the sounds had always been there, but the stakes were higher since I was the only one in the cockpit doing it without the safety of my instructor. My CFI had a good laugh and I thought about this situation during our training.

When you first go solo at home, you will hear “new sounds and alarms” but do not be frightened, you will get used to it. Then the question arises, “who does what when?” We tend to have a nice rhythm with one another and our treatment days go something like “I’m going to start my arm” which means she is going to prepare her arm, apply the numbing cream and start priming the machine. I am fully capable of putting in the cartridge, priming the machine (and I think this machine has a soul and some days just feels like being a trouble maker) but she likes to do it. We started doing it this way because it gives her something to do while she waits (she is not known for her patience or sitting still), and she is very independent so prefers for “her treatments” to be “responsible for the work, since she is a burden.” This is not true of course, but because of her thinking, she usually will start that process. During this time, she also gets her supplies ready, tape ready, the syringes, and everything else she needs when treatment begins. Perhaps in your situation, you will do all of the setup, there is no right or wrong answer, so long as it gets done.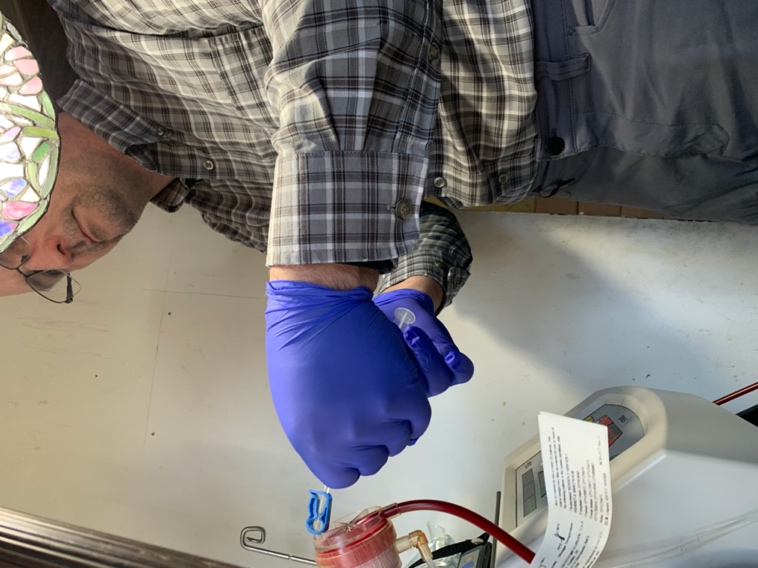
The next thing that is usually heard (unless the machine is in a bad mood and decides to alarm) is “I’m going to wash my warm now,” which means she is going to actually wash her arm and that treatment is about to begin. This tells me it is time for me to get ready for my job. Some days, if we are doing the ole’ “hanging bags trick”, I am hanging the bags, getting the lines connected and the like. If we are using the PureFlow®, then I am making sure the temperature is set. At least one day before this, I have made sure that a SAK is ready, solution tested, and the like. Sometimes she remembers to do it, sometimes I remember to do it, sometimes as we are falling asleep panic washes over one of us because we remember that we forgot to make a batch, but between the two of us, most of the time it is remembered.
As she sanitizes her arm, I am connecting the bags, or treatment lines to the PureFlow, making sure she has flipped the cartridge, and double checking the supplies. I do not have to check her, but on occasion she forgets things and so do I. As I am setting the machine parameters, she is double checking that I have not missed it while she is sanitizing her arm and preparing to cannulate (put her needles in). As I am waiting on her to be ready for me to hand to her the lines, I am double checking the machine numbers, line clamps, and supplies. Is the Epogen already prepared and in the refrigerator? Has she prepared the heparin? Does she have gloves, tape, gauze? These are ways, without saying a word that we double check one another.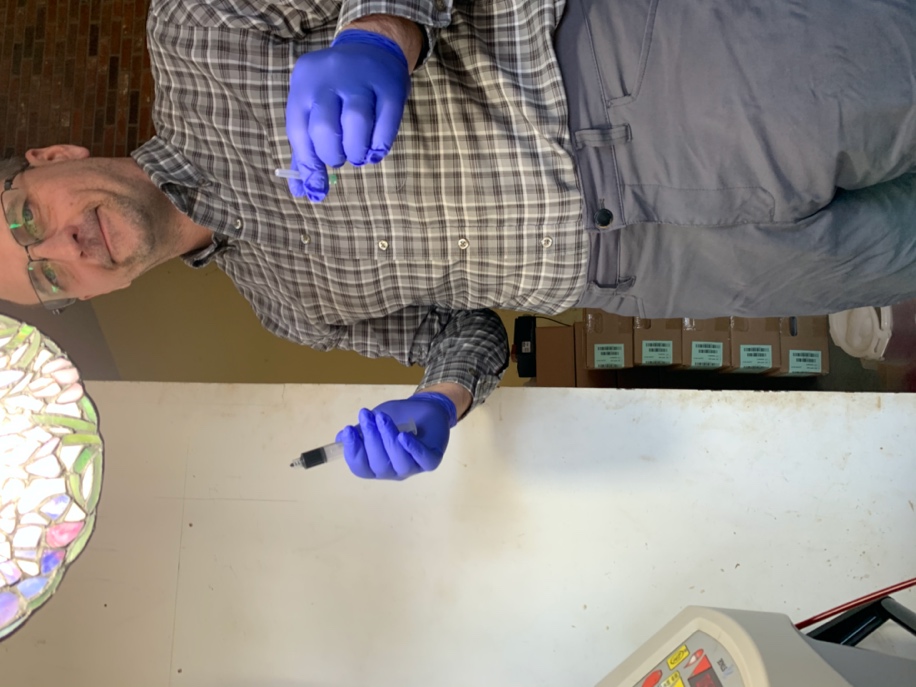
During treatment, when that machine decides it wake up in a bad mood and beeps constantly, we are both determining what the error is and how to resolve it. Is it air? I know that is my cue to get the “big syringe” and pull air. Is it, as is common, a flow problem? That is my cue that I need to double check the clamps, because I probably didn’t unclamp the green one. After treatment, her habit is the lay out her tape and gauze about 10 minutes before treatment ends, so when I see her laying out the tape, I know it’s about time for me to get to work. I grab the Epogen and have it ready (she often never even thinks to ask me to because I just know that is going to be needed soon—she would get it but the lines are a little short and they frown on getting up during treatment) and then get ready for ending treatment. I have prepared the saline for the flush, and on a good day, take her lines and reconnect to the saline bag and then discard her needles as she removes them. On a bad day, I add “grabbing more gauze fast to stop the bleeding.”
In the end, we tried various methods and somehow magically settled on the process that we have. I now know by the sound of the machine about how much time remains. I know by her attitude, how supportive and encouraging that I will need to be or how much double checking that I will need to do. My heartbeat does not increase if her BP gets too low, the machine beeps, and I cannot remember the last time I had to look at the book to know what the next steps were.
I promise, you REALLY DO have this. I believe in you. Your team believes in you, your partner (hopefully) believes in you, and you CAN do this. We have been described as a symphony with a perfect balance of melody and harmony (no pun intended, her name really is Melody), and our system has a great ebb and flow. This did not happen the first time we were solo at home nor did it happen quickly. There were days of frustration, anxiety, and today there are times when events occur that are scary. For example, last week her BP dropped to a number I will not type for her doctor to see and she was on the verge of passing out. However, because of our symphony and training, I knew what to do, knew how to do it, and all without a word spoken. You will develop your pattern and rhythm but convince yourself that you CAN do this and over time you will find the right “flow” for your PureFlow.



Comments
Elizabeth
Jan 19, 2021 11:00 AM
Ann Contreras
Jan 18, 2021 10:00 PM
Thank you! Thank you! Thank you!
David L. Rosenbloom
Jan 18, 2021 6:18 PM
Paz Moscovitch Gun-Zakh
Jan 18, 2021 6:11 PM
How many years you do it at home? we are the only one in our country that doing HHD (Israel) God Bless you
Courtney
Jan 18, 2021 5:26 PM
I’m my mothers care partner. She cannot do it for herself at all. I am in the medical field and I was terrified of doing dialysis for her at home. It’s still sometimes nerve racking due to her Health situation and she passes out a lot.But yes you definitely find your flow with your pure flow😊