Medicare Advantage Plan Pros & Cons—and a Fix for Buyers’Remorse


Dialysis and Health Insurance Discrimination
Dialysis patients have faced health insurance discrimination for decades, because ESRD is a pre-existing condition. Federal law gives people 65 and older guaranteed rights to buy a Medigap plan from any company without regard to their health. The clock starts when they get Part B. But, several states have no regulations to provide similar protections to those under age 65 who are on dialysis. To avoid large bills, they need to have coverage from a job or be eligible for Medicaid or one of the Medicare Savings Programs that helps pay out-of-pocket costs.
Dialysis companies and kidney organizations lobbied to give dialysis patients the option to join a Medicare Advantage (MA) plan. Dialysis patients were informed last year that they could enroll in any MA plan from October 15 through December 7, and the plan would take effect on January 1, 2021. Some were excited to hear this. Patients who may not have experience reviewing health plans found themselves having to choose from multiple plans. Many reached out to others to help them decide. It was a big responsibility for those helping to make sure they reviewed the advantages and disadvantages so as few patients as possible would experience unforeseen problems in the choice they made.
Medicare Costs in Original Medicare and MA Plans
Original Medicare has no cap on how much an individual could owe in out-of-pocket costs for deductibles, coinsurance, and copays. MA plans are required to cap those costs:
-
In 2021, an MA plan member cannot be required to pay more than the CMS mandated maximum out-of-pocket (MOOP) of $7,550 for in-network Part A and B services.
-
The CMS mandated maximum for in- and out-of-network Part A and B services (when plans cover out-of-network services) is $11,300 in 2021.
-
Plans can choose to set a lower cap, and some have done that.
-
Drug costs are not under those caps.
Types of MA Plans Sold by Private Insurance Companies in 2021.
The Medicare site describes four types of MA plans:
-
Health Maintenance Organizations (HMOs) require members to get all care from in-network providers. These plans will not pay for out-of-network care except for urgent care or emergencies and out-of-network dialysis. Patients usually need a referral from a primary care doctor to see a specialist. If a doctor leaves the network, the patient must get another one in the network. MA HMOs cover drugs on their formulary.

-
Preferred Provider Organizations (PPOs) let members seek care in- or out-of-network. PPOs pay more for care patients get in-network, and may limit care to within a certain local area or region, except for urgent or emergency care. Most offer drug coverage, but if not, the patient cannot get a separate Part D plan.
-
Special Needs Plans can be HMOs or PPOs. These serve certain people, like those in nursing homes with Medicaid or with certain medical conditions, like diabetes, HIV, ESRD, etc. Members may have to have a primary care provider and get a referral to see other providers. They must stay in-network unless in an emergency or for out-of-network dialysis. These plans have drug coverage.
-
Private Fee-for-Service plans allow members to see any doctor or hospital that accepts their plan. Patients should make sure each provider accepts their plan before making an appointment. If the plan has a network, it will pay more for care the patient gets in-network. Patients can get care from any doctor or hospital in an emergency.
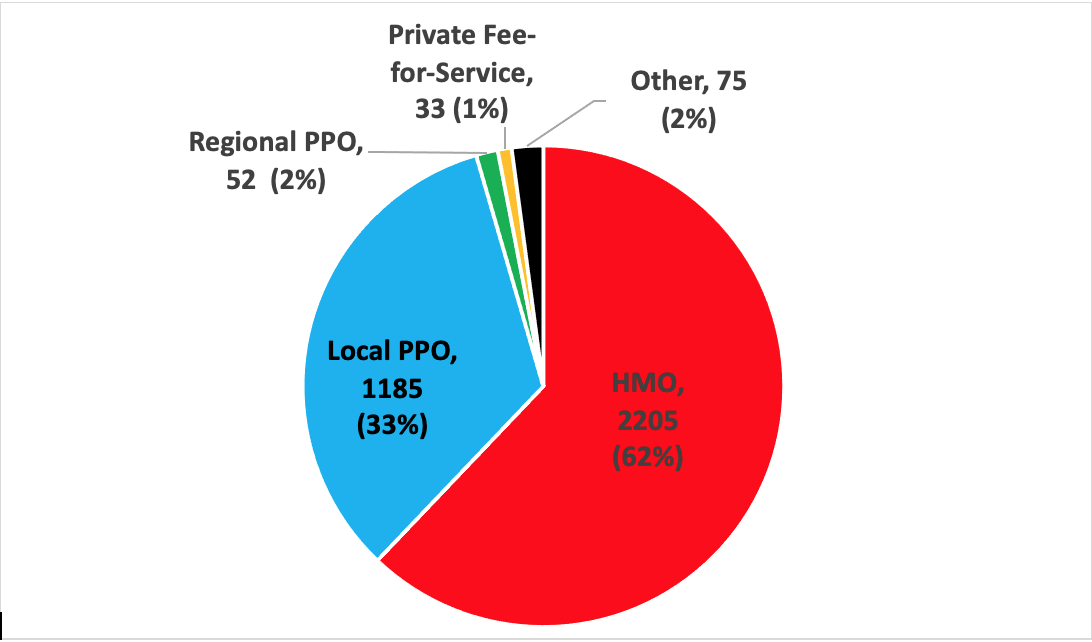
In 2021, there are 3,350 MA plans.1 These are the number of plans of each type except Special Needs plans or MA plans offered through employers:
Advantages of MA Plans
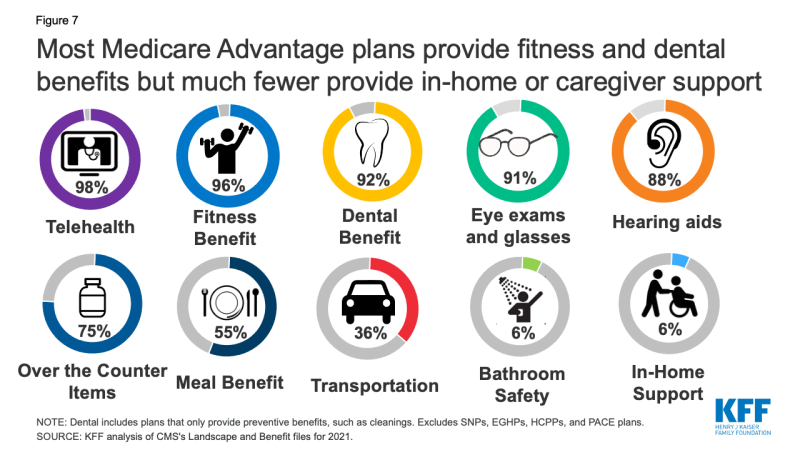
Drug coverage is available in 89% of MA plans and 54% of those MA plans have no premium over the monthly Part B premium. Nationwide, 96% of Medicare beneficiaries had a choice for 2021 of at least one MA plan with no extra premium. Advertisements showed MA plans’ extra benefits that Original Medicare does not offer. Patients should read their plan policy to see if there are limits on these benefits, or if they have an extra cost.
Disadvantages of MA Plans
People who develop kidney failure may have already had an MA plan or switched to one this year. If their doctor, hospital, dialysis clinic, or transplant program is not in-network, they may have to switch providers to get the plan to cover the cost or to do so at the best rate. Depending on a plan’s network, a patient may have to travel farther to get the service they want—or go to a provider who has a lower rating. Some transplant candidates have found that although their nephrologist and dialysis clinic are in-network, the transplant hospital they were working with is not.
One of the biggest drawbacks with MA plans is that a Medigap plan with Original Medicare may no longer work with an MA plan someone switched to. And, if a patient drops a Medigap plan, s/he may not be able to get it back later.

There May Be a Fix for Those New to Medicare and an MA Plan in 2021:
On page 74 of the Medicare & You booklet it says:
“If you join a Medicare Advantage Plan for the first time, and you aren’t happy with the plan, you’ll have special rights under federal law to buy a Medigap policy and a Medicare drug plan if you return to Original Medicare within 12 months of joining the Medicare Advantage Plan.
-
If you had Medigap before you joined, you may be able to get the same policy back if the company still sells it. If it isn’t available, you can buy another policy.
-
If you joined a Medicare Advantage Plan when you were first eligible for Medicare (and you’re not happy with the plan), you can choose from any Medigap policy within the first year of joining.
-
Some states provide additional special rights to buy a Medigap policy.
Note: If you don’t drop your Medicare Advantage Plan and return to Original Medicare within 12 months of joining, generally, you must keep your Medicare Advantage Plan for the rest of the year. You can disenroll or change plans during the Open Enrollment Period or if you qualify for a Special Enrollment Period. Depending on the type of Special Enrollment Period, you may or may not have the right to buy a Medigap policy.”
Patients who are unhappy with their MA plan can switch to a different MA plan or to Original Medicare from January 1 through March 31 each year, and the plan will start the next month. They can switch again during open enrollment from October 15-December 7, and that plan will start the following January.
 ALERT: Patients who joined an MA plan as their first option for Medicare or switched to an MA plan can only get a Medigap plan when they switch out of their MA plan if they have been in that plan for 12 months or less. If they are under 65 and on dialysis, they can only get a Medigap plan if their state offers Medigap plans to people their age on dialysis. The first time to switch plans or switch back to Original Medicare is March 31. This deadline is coming up soon. Patients who are thinking about changing plans may want to talk with their state health insurance assistance program. These counselors are unbiased and are not paid by an insurance company, so will counsel—but not steer—people into any plan.
ALERT: Patients who joined an MA plan as their first option for Medicare or switched to an MA plan can only get a Medigap plan when they switch out of their MA plan if they have been in that plan for 12 months or less. If they are under 65 and on dialysis, they can only get a Medigap plan if their state offers Medigap plans to people their age on dialysis. The first time to switch plans or switch back to Original Medicare is March 31. This deadline is coming up soon. Patients who are thinking about changing plans may want to talk with their state health insurance assistance program. These counselors are unbiased and are not paid by an insurance company, so will counsel—but not steer—people into any plan.
1 Biniek JF, Freed M, Damico A, Neuman T. Medicare Advantage 2021 Spotlight: First Look. Kaiser Family Foundation. October 29, 2020. https://www.kff.org/medicare/issue-brief/medicare-advantage-2021-spotlight-first-look/


Comments
Beth Witten
Sep 18, 2021 2:55 PM
Lucy Huerta
Sep 18, 2021 11:31 AM