Medicare May Be Better than a Marketplace Health Plan

Normally, open enrollment for Marketplace health plans is from November 1 through December 15 unless someone has a
reason for a special enrollment period. However, with many lost jobs and coverage due to COVID-19, the Biden
Administration re-opened enrollment from February 15 - May 15, 2021. This is a good
thing for people who do not have and cannot get health insurance any other way. Below is a map from
the Kaiser Family Foundation1 showing plans in the U.S.:
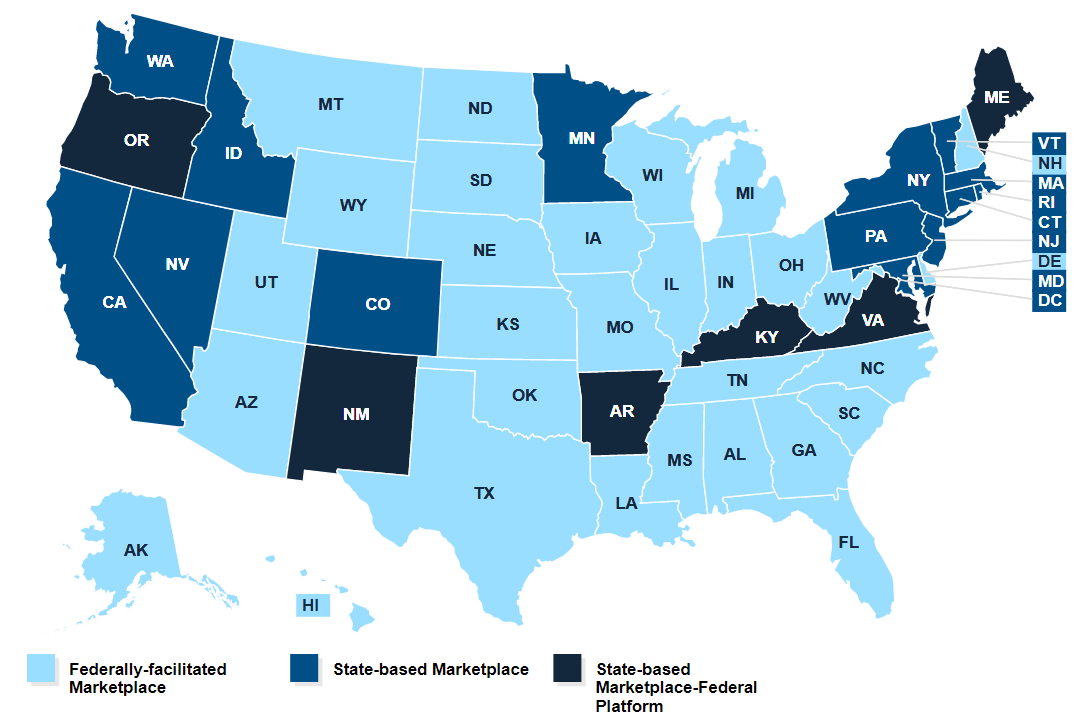
Here is how the Kaiser Family Foundation describes the plans:
-
“State-based Marketplace (SBM): States running a State-based Marketplace are responsible for performing all marketplace functions for the individual market. Consumers in these states apply for and enroll in coverage through marketplace websites established and maintained by the states.
-
State-based Marketplace-Federal Platform (SBM-FP): These states are considered to have a State-based Marketplace, and are responsible for performing all marketplace functions for the individual market, except that the state will rely on the federal Healthcare.gov website for eligibility and enrollment functions. Consumers in these states apply for and enroll in coverage through Healthcare.gov.
-
Federally-facilitated Marketplace (FFM): In a Federally-facilitated Marketplace, HHS performs all Marketplace functions. Consumers in FFM states apply for and enroll in coverage through Healthcare.gov.”

Seven Reasons WhyOriginal Medicare May be Better than a Marketplace plan
-
Dialysis clinics are limited in what they can charge Original Medicare. Their charges include dialysis (in-center and home), staff time, dialysis-related drugs and lab tests, and most supplies, including access dressings and coverings for bathing for in-center or home patients, a stand-on or wheelchair scale if a patient can’t stand, and an adjustable chair for home patients. In 2021, Medicare’s base payment rate for dialysis is $253.13.
-
Dialysis clinics can charge Marketplace plans many times what Medicare allows, and they can bill separately for lab tests, drugs, supplies, etc. that a clinic must provide under the ESRD prospective payment rate (bundle) for those with Original Medicare.
-
 Marketplace plans have large deductibles and copays or coinsurance.
Although some patients receive subsidies to help them pay, those who make too much to qualify for these
subsidies could owe a lot more. If patients provide a statement about their finances, dialysis clinics may
discount bills—but non-dialysis providers may not.
Marketplace plans have large deductibles and copays or coinsurance.
Although some patients receive subsidies to help them pay, those who make too much to qualify for these
subsidies could owe a lot more. If patients provide a statement about their finances, dialysis clinics may
discount bills—but non-dialysis providers may not. -
Most Marketplace plans have networks that limit who patients can see or where they go, including their ability to seek non-emergency care (except dialysis) out of network when traveling. With Original Medicare a patient can go to any doctor or other provider that accepts Medicare. Even if people go to a network hospital, they can get surprise bills if a doctor is not in-network. This happens with job-based insurance plans too.
-
Marketplace plans change network providers from time to time, which can mean giving up a trusted relationship with a doctor, dialysis clinic, or transplant program. This change can be upsetting and can affect continuity of care.
-
After their initial enrollment period, patients can enroll in Medicare only during the general enrollment period of January through March each year, if they keep an individual (non-job-based) Marketplace plan when they start dialysis or get a transplant. Medicare will not start until July 1. And, patients may owe a premium penalty monthly until they are eligible for Medicare due to age or another disability.
-
Patients who do not have Medicare Part A the month of their transplant can never use Part B to pay for immunos for that transplant—even if they get Medicare later due to age or disability. NOTE: A new law passed in 2020 that starts January 1, 2023 extends Part B immunos only for those had Medicare coverage for immunos, but lost it 36 months post-transplant and have no other health plan. Those who kept their Marketplace plan are not eligible for this new benefit.
A few questions to ask patients:
-
 Do you see or want to see a provider or hospital that is not in the Marketplace plan’s network?
A plan may not provide notice of a change of providers at a time when the patient can
change Marketplace plans (the fall).
Do you see or want to see a provider or hospital that is not in the Marketplace plan’s network?
A plan may not provide notice of a change of providers at a time when the patient can
change Marketplace plans (the fall).
-
Do you like to travel? Ask the patient to anticipate whether s/he could see possibly needing routine care other than dialysis while away from home.
-
Do you want a transplant? The transplant program would need to be in-network for the patient. If someone gets AKF help to pay Marketplace premiums, a transplant program may expect him or her to raise funds to show ability to pay plan premiums without AKF help.
Conclusion
The Affordable Care Act has been challenged in Congress and in the courts, and could be again, which could eliminate Marketplace plans and leave patients stranded until their Medicare enrollment period. People who work for Medicare have said that Medicare is better than a Marketplace plan for those who can get it. Patients who live in a state where they can supplement Medicare with a Medigap plan or Medicaid will likely save money over coverage in a Marketplace plan. If a patient is in a Marketplace plan that is not working well, s/he needs to know that Medicare enrollment is limited, won’t start until July, and premiums may be higher for late enrollment. An income eligible patient can keep Marketplace premium tax credits and subsides until Medicare Part A starts.2,3
1 Kaiser Family Foundation. State Health Insurance Marketplace Types, 2021.https://www.kff.org/health-reform/state-indicator/state-health-insurance-marketplace-types
2 Changing from the Marketplace to Medicare. https://www.healthcare.gov/medicare/changing-from-marketplace-to-medicare/
3 Medicare and the Health Insurance Marketplace. https://www.medicare.gov/Pubs/pdf/11694-Medicare-and-Marketplace.pdf


Comments
Mary Beth Callahan
Apr 19, 2021 1:02 AM
Lisa M Hall
Mar 18, 2021 9:00 PM