In-center HD Complaints that Could be Solved by Going HOME


While standard in-center HD comes with predictable set of gripes I’ve heard hundreds (thousands?) of times over the years, many dialyzors seem to have a sort of “better the devil you know” approach. Rather than consider switching to a type of dialysis that might improve day-to-day life, or in some cases, make it worth living at all, the main focus seems to be the dream of a transplant—which could be years away—plus a large dose of fatalism.
I’ve found and deidentified several typical quotes from social media that are examples of these gripes. For each one, I’ll briefly explain how choosing a home option can help. This post is both for people who might want a better life and to help sensitize dialysis staff to the lifestyle impact of the “default” treatment option.
“Today, I'm really struggling. There's so many appointments that have been scheduled for me, I don't know how to deal with it all, especially on top of having to do dialysis 3 times a week and physical therapy on the days I don't have dialysis. How can I keep myself from getting overwhelmed?”
Think about when you go to the doctor or dentist. You spend time in the waiting room, and then in a treatment room, before you even see the doctor. A 10-minute appointment can take hours, by the time you drive there, complete the forms, wait, wait some more, see the doctor, perhaps pick up a prescription, and drive home.

Now, imagine having a 3+ hour long appointment three times each week, plus travel time, driving, and, often, feeling pretty lousy for hours afterward. How would you fit in grocery shopping? Physical therapy visits? The kids’ soccer practice? A job—so you can have a health plan and keep a roof over your head and the lights on and buy food? (Disability may pay only 1/3 as much as work did; it’s not a good solution for someone with a mortgage to pay off.)
We often don’t give a thought as to what standard in-center HD does to people’s daily routines. The message seems to be, “Suck it up, you’d die without this.” No inconvenience is too great—for someone else—just as the dialysis needles don’t hurt when they’re not in your own arm.
PD and home HD can give people back control of their time. Yes, the treatments must be done. But, it’s far more possible to fit life in around them when you can choose the days and the times.
“I have a new, radical idea regarding the frequency of the dialysis offered to me by the for-profit dialysis companies available to me. How about offering dialysis to patients when they need it instead of when it works for them? I need dialysis every other day to feel my best—not three times a week. I feel bad every Sunday, and I cannot find any dialysis center that provides this. Why??”
Why, indeed? Thrice weekly in-center HD is a historical accident. In the early days of dialysis in Seattle, nephrologists (the term had not yet even been coined) experimented with the number of days of treatment, since there were not enough machines and supplies to treat everyone. One day of dialysis per week: people died. Two days of dialysis per week: people died. But, at three days, people lived—some for decades. (NOTE: Those first dialysis treatments were 8-12 hours long, and this matters!). Every-other-day or more frequent HD were not tried at the time, and when Medicare started to pay for dialysis in 1993, it codified the thrice weekly schedule without saying how long treatments had to be (an epic mistake, in my opinion).
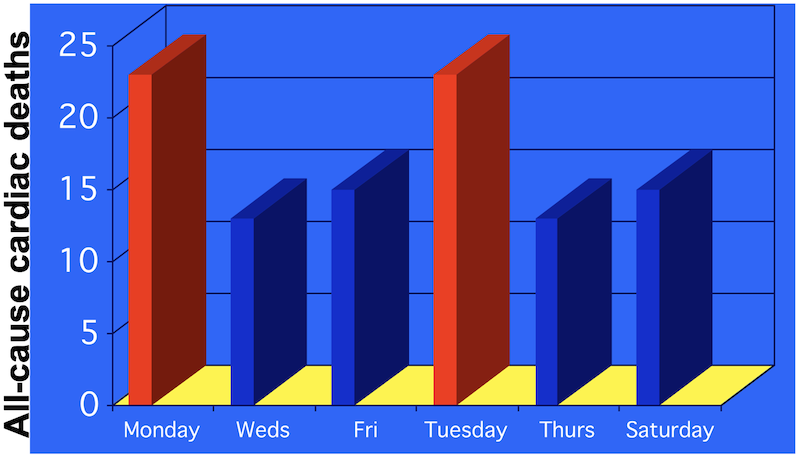 Since then, studies have looked at survival on standard in-center HD by days of the week. On PD, survival is the same each day. But, in 1999, Bleyer et al did a study of all of the 375,482 U.S. deaths on dialysis from 1977 to 1997.1 What they found was shocking. “For all hemodialysis patients, Monday and Tuesday were the most common days of sudden and cardiac death.” In fact, while 14.3% of deaths would have been expected if the distribution was the same every day, the rate was 20.2% on Mondays (and similar on Tuesdays)—a 41.25% increase.
Since then, studies have looked at survival on standard in-center HD by days of the week. On PD, survival is the same each day. But, in 1999, Bleyer et al did a study of all of the 375,482 U.S. deaths on dialysis from 1977 to 1997.1 What they found was shocking. “For all hemodialysis patients, Monday and Tuesday were the most common days of sudden and cardiac death.” In fact, while 14.3% of deaths would have been expected if the distribution was the same every day, the rate was 20.2% on Mondays (and similar on Tuesdays)—a 41.25% increase.
So, the day after the 2-day no-treatment gap does not just make people “feel bad every Sunday,”—it can be lethal. Other population research has found the same thing.2
Dialysis clinics could go to an every-other-day schedule. But, not easily. Schedule logistics and transportation for a 2-week schedule of alternating days would be a nightmare. People would forget which days they needed to be there. At home, though, it is easy to dialyze every other day—or to do 4 or 5 or 6 days or nights. No more feeling bad on Sundays.
“I am 26 years old have been on dialysis for 4 years now. I am addicted to ice and will stop at nothing to get it. I've been looking for other things to get my mind off ice, but nothing has worked yet. My Mom and I have the same fight over and over again because we can't seem to agree on anything when it comes to my fluid.”
Two things are top of mind for driving ice cravings:
1). Fluid limits—especially if people are rescued from blood pressure crashes with saline, which triggers the thirst drive in the brain. This is a topic Dr. John Agar has blogged about extensively here at KidneyViews.3 Besides fluids, complex diet limits can turn a simple pleasure like eating into angst-ridden avoidance that can even lead to malnutrition.
2). Pica (a craving for ice or non-food substances, such as laundry starch, dirt, or clay. Pica can be triggered by anemia.
Either or both of these could be going on. In-center, longer treatments could help.2 A better solution, for those who can do it, is to do a home treatment. Any option besides standard in-center HD will allow for more gentle water removal and therefore permit a bit (or a lot) more freedom in fluid intake.
With fewer toxins in the blood, red blood cells can survive longer, too. This may be one reason why people who do short daily or nocturnal home HD need less erythropoietin to control anemia.4,5
“Help there's a tech that always has jokes very disrespectful check my purse take my shoes off throw it when I'm holding my site he push my hand away that can make me bleed all a joke I smack him once and told him is not fun anymore 3 times a week like it's funny what can I do.. he don't wanna stop?”
Harrassment by dialysis staff during a life-saving treatment is terrifying for someone trapped in a chair, with blood passing through tubing, and life in the hands of a “joker.” A clinic should not tolerate any type of unprofessional behavior. It is difficult to understand why other staff would not stop this, but it does happen. In clinics. Where doesn’t this happen? At home.
“Does anyone else's body give them a signal that it's time to stop when finding your dry weight? Today I had a 1 hour UF treatment before my regular one to get back to dry, but I think I gained actual weight. Now I just feel like a crampy, wrung out towel. My neck gets the twinges and that's my tell to stop treatment. It was 35 minutes early today. I rarely sign off like that. I knew it was coming though. As soon as I got to my car, the neck twinges exploded into full blown, pulling my head to the right, cramps. Joy. A few minutes later I drive the whole 2 miles home. By the time I get to my apartment with my pillow and pocketbook, my left leg started twinging...and cramped hard for a solid hour. I really wish there was an easier way to figure your weight when it shifts. They have critlines and all that jazz but I really don't think it's as accurate as they say.”
Cramps, cramps, cramps. We have “normalized” these in the U.S. People expect to cramp. Cramping is just part of dialysis, right?
Wrong! I would argue—and often do—that cramps are common, but not normal. They should be a never event.
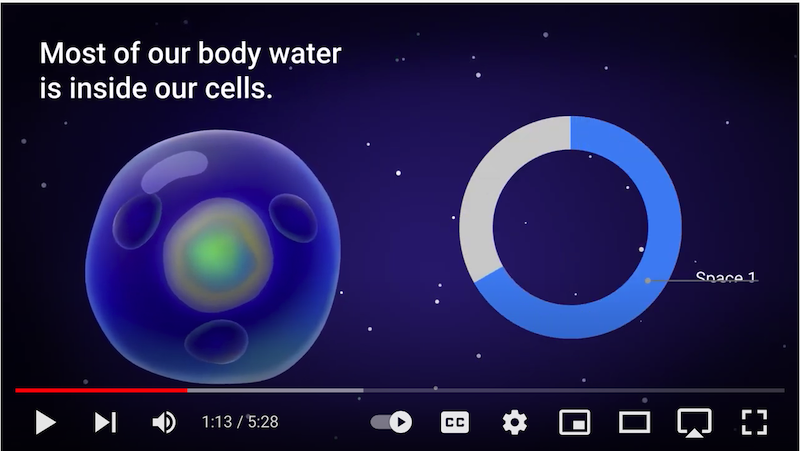
Why? Cramps occur when blood pressure drops (intradialytic hypotension, or IDH), and blood pressure drops when too much water is removed, or water is pulled out of the bloodstream faster than the transcapillary refill rate can replenish it (just 2-6mL/Kg/hour).6 IDH can stun the heart,7 brain—affecting cognitive function,8 gut,9 and any remaining kidney function10 by starving them of oxygen-carrying red blood cells. Our handy 5-minute video shows you how this works. Myocardial (heart muscle) stun, in particular, is a factor in sudden cardiac death.7 The earlier IDH occurs in a treatment, the deadlier it seems to be.11
Standard in-center HD can be made safer by:
Encouraging people to not gain too much water weight, and to limit salt and sugar.
Doing slower, gentler ultrafiltration (UF). Unfortunately, while Medicare attempted to enforce gentler UF rates by limiting clinics to less than 13 mL/Kg/hour, this is still far too high—more than twice the upper limit of the transcapillary refill rate.
Using our free Ultrafiltration Rate Calculator at each treatment to stay in the green.
Cooling dialysate to about ½°C below core body temperature (34° to 35.7°C) can reduce IDH by 70%.12
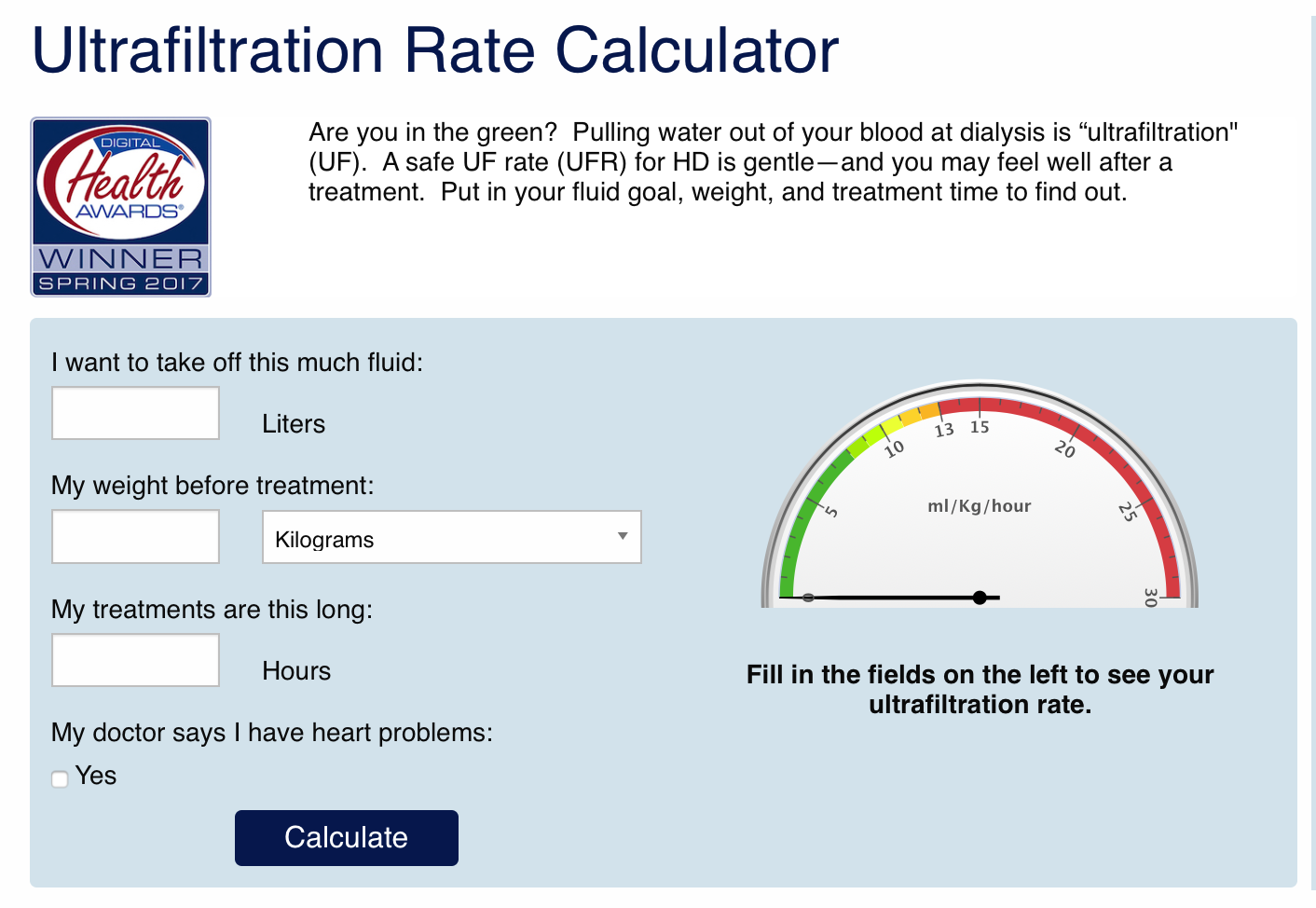
At home (where this calculator is also useful for HD), water can be removed every day with PD, or longer and/or more frequent treatments can be done with HD to prevent IDH, cramps, and stunning.
“My cramps are out of control and it's miserable to be woken up with a cramps that won't stop!! I'm taking 7 Lasix, 2 metolazone and 2 spironolactone daily. My doctor has told me to take Biotin, magnesium and Hyland leg cramps pills, but I'm still having them almost every night! They gave me Gabapentin for my back and the cramps on Monday...but I'm still having them. Plus, my back pain isn't any better on them either! Does anyone have any suggestions??? Can anyone tell me if I stop treatment, is it slow and painful or quick and painless? I know it's not what people want to think or talk about but I would really honestly like to know. Please don't judge!!!”
There is another risk of cramps, besides physical damage to the heart: loss of the will to live. Is a life full of daily miseries worth living if there are no compensating joys? This is, obviously, an intensely personal question. But, each year, many Americans on standard in-center HD say no, and they withdraw from treatment.
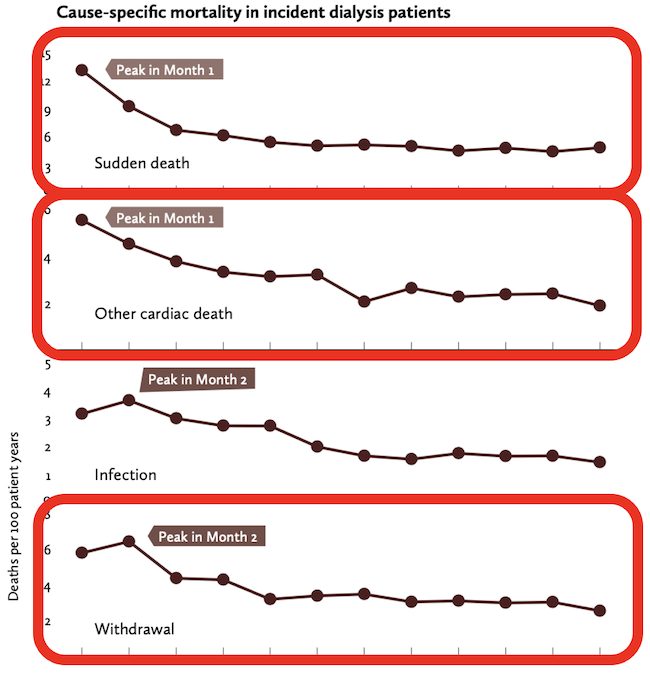
We have known for nearly a decade that the first few months of standard in-center HD are dramatically more deadly than later ones.13 To me, this graph—from the PEER report, a reanalysis of USRDS data14—has always told a powerful story.
Sudden death and other cardiac death peak in month 1. Withdrawal from dialysis (for survivors) peaks in month 2. So, what I see is that after a terrifying month of an intrusive therapy that makes many feel worse instead of better, they may just say, “Why am I doing this?!” —and stop. You might do the same.
Not everyone is a candidate for a home therapy. About 13% of people are not physically suited for PD, found a prospective study.15 Housing and storage are considerations for any home therapy. And, while PD and daily home HD can be done solo, some do not feel comfortable without a partner, and either don’t have one or have one who is actively opposed to taking on a partner role or having equipment in the home. For those who can, doing some form of home dialysis can improve day-to-day quality of life, enhance the chance of a transplant (by demonstrating self-management), and perhaps even save their own lives.
Bleyer AJ, Russell GB, Satko SG. Sudden and cardiac death rates in hemodialysis patients. Kidney Int. 1999;55:1553-1559↩︎
Zhang H, Schaubel DE, Kalbfleisch JD, Bragg-Gresham JL, Robinson BM, Pisoni RL, Canaud B, Jadoul M, Akiba T, Saito A, Port FK, Saran R. Dialysis outcomes and analysis of practice patterns suggests the dalysis schedule affects day-of-week mortality. Kidney Int. 2012 Jun;81(11):1108-1115↩︎
Agar J. Towards compassionate dialysis: thirst and hemodialysis duration. KidneyViews blog post, April 7, 2016. https://homedialysis.org/news-and-research/blog/146-towards-compassionate-dialysis-thirst-and-hemodialysis-duration.↩︎
Roblero MFS, Rubio MAB, Gonzalez-Moya M, Varela JC, Alba AJ, Gumpert JV, Cigarran S, Vidau P, Marcos SG, Luquin PA, Piera EC, Marino AG, Espigares MJ, Molina MD, Molina P. Experience in Spain with the first patients in home hemodialysis treated with low-flow dialysate monitors. Nefrologia. 2021 Aug 12;S0211-6995(21)00144-2↩︎
Burton JO, Graham-Brown MPM. Nocturnal hemodialysis: an underutilized modality? Curr Opion Nephrol Hypertens. 2018;27:472-477.↩︎
Mitsides N, Pietribiasi M, Waniewski J, Brenchley P, Mitra S. Transcapillary refilling rate and its determinants during haemodialysis with standard and high ultrafiltration rates. Am J Nephrol. 2019 Jul 9;50(2):133-143↩︎
Burton JO, Jefferies HJ, Selby NM, McIntyre CW. Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol. 2009;4:914-920↩︎
Findlay MD, Dawson J, Dickie DA, Forbes KP, McGlynn D, Quinn T, Mark PB. Investigating the relationship between cerebral blood flow and cognitive function in hemodialysis patients. J Am Soc Nephrol. 2019;30:147-158↩︎
McIntyre CW. Haemodialysis-induced myocardial stunning in chronic kidney disease – a new aspect of cardiovascular disease. Blood Purif. 2010;29:105-110↩︎
Marants R, Qirjazi E, Grant CJ, Lee T-Y, McIntyre CW. Renal perfusion during hemodialysis: intradialytic blood flow decline and effects of dialysate cooling. J Am Soc Nephrol. 2019;30:1086-1995↩︎
Keane DF, Raimann JG, Zhang H, Willets J, Thijssen S, Kotanko P. The time of onset of intradialytic hypotension during a hemodialysis session associates with clinical parameters and mortality. Kidney Int. 2021;99:1408-1417↩︎
Mustafa RA, Bdair F, Akl EA, Garg AX, Thiessen-Philbrook H, Salameh H, Kisra S, Nesrallah G, Al-Jaishi A, Patel P, Patel P, Mustafa AA, Schunemann HJ. Effect of lowering the dialysate temperature in chronic hemodialysis: A systematic review and meta-analysis. Clin J Am Soc Nephrol. 2016;11:442-457↩︎
Robinson B, Zhang J, Morgenstern H, Bradbury BD, Ng LJ, McCullough K, Gillespie B, Hakim R, Rayner H, Fort J, Akizawa T, Tentori F, Pisoni R. World-wide, mortality is a high risk soon after initiation of hemodialysis. Kidney Int. 2014 Jan;85(1):158-165↩︎
Peer Kidney Care Initiative, Peer Report: Dialysis Care and Outcomes in the United States, 2014, Chronic Disease Research Group, Minneapolis, MN, 2014.↩︎
Mendelssohn DC, Mujais SK, Soroka SD et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol Dial Transplant. 2009 24:555-61↩︎


Comments
Dori Schatell
Sep 29, 2021 2:34 PM
John Agar
Sep 23, 2021 10:56 PM
Please, some of you out there, read, listen, act, to change this.
Leong Seng Chen
Sep 23, 2021 8:23 PM