Involuntary Dialysis Clinic Discharges: Can More Be Avoided?

Background
I recently read a post from a PD patient on the Home Dialysis Central Forum who was involuntarily discharged (IVD) from his clinic and couldn't find another one willing to accept him. I've heard from a hospital social worker trying to place two patients who were getting emergency dialysis in her hospital. Despite not missing any treatments and no behavior issues for months, she couldn't find a clinic willing to admit them. Her patients were getting regular treatments three times weekly, but most patients who experience IVD get emergency dialysis only when their labs show an emergent need. They are at high risk of dying. In 2014 after reading multiple posts from members of the Home Dialysis Central Facebook group, I wrote a post entitled Involuntary Discharge: What Happened To The Oath “First, Do No Harm”? This post revisits this life and death topic.
ESRD Conditions for Coverage and Interpretive Guidance
In that 2014 post, I shared text from the ESRD Conditions for Coverage from the Condition for Patients' rights, including the patient's right to refuse treatment. I also shared text from the Condition for Plan of care about when goals and targets aren't met. The following quote is from the Interpretive Guidance CMS shares with surveyors to help them better understand what the regulation text means, so they can see if a dialysis clinic is complying with the regulations:
“The IDT must recognize each patient has the right to choose less than optimal care when the patient determines optimal care would negatively impact his/her quality of life…These regulations require the IDT to demonstrate its members are actively attempting to meet each patient's plan of care goals. This Condition does not 'require' a patient to meet every goal. Any member of the IDT, including the patient, may document why goals are not met or cannot be met.”

I wonder if reading this quote may help dialysis staff recognize that they can't control a patient's behavior and their attempts to address behavior are often seen by patients as nagging. How many of us can admit that nagging triggers our anger, acting out, and even aggression? How many conflicts between patients and dialysis staff that put patients at risk of involuntary discharge (IVD) started with staff trying to get a patient to do what that staff sees is in the patient's best interest? A patient needs to be encouraged to be actively involved in developing his/her plan of care and reporting barriers to following that plan. If that doesn't happen, staff can't identify and address barriers or even help the patient see how meeting clinical goals and targets can help meet their goals for living their best life in spite of dialysis.
Under the Conditions for Governance states the allowed reasons for IVD. The Interpretive Guidance states:
“Involuntary discharge or transfer should be rare and preceded by demonstrated effort on the part of the interdisciplinary team to address the problem in a mutually beneficial way. The facility must have and follow written policies and procedures for involuntary discharge and transfer… Patients should not be discharged for failure to comply with facility policy unless the violation adversely affects clinic operations (e.g., violating facility rules for eating during dialysis should not warrant involuntary discharge). Patients should not be discharged for shortened or missed treatments unless this behavior has a significant adverse affect (sic) on other patients' treatment schedules. A facility may evaluate the patient (who shortens or misses treatments) for any psychosocial factors that may contribute to shortening or missing treatments; for home dialysis; or, as a last resort to avoid inconveniencing other patients, may alter the patient's treatment schedule or shorten treatment times for patients who persistently arrive late.. Patients should not be discharged for failure to reach facility-set goals for clinical outcomes.”
Tracking Data on IVD
ESRD Networks report and track patient grievances and IVDs. The End Stage Renal Disease Network Organization Program 2002 Summary Annual Report reported 404 IVDs. The End Stage Renal Disease (ESRD) Network Program 2019 Summary Annual Report didn't report IVDs separately. The report said there were 1,067 “access to care” reports that year, which includes:
At risk for involuntary discharge or involuntary transfer
Scheduled for or experienced IVD or IVT
No access to an outpatient clinic or Failure to Place
Behaviors
Medical Needs
Non-payment Issues
Facility Refusal/Failure to Place

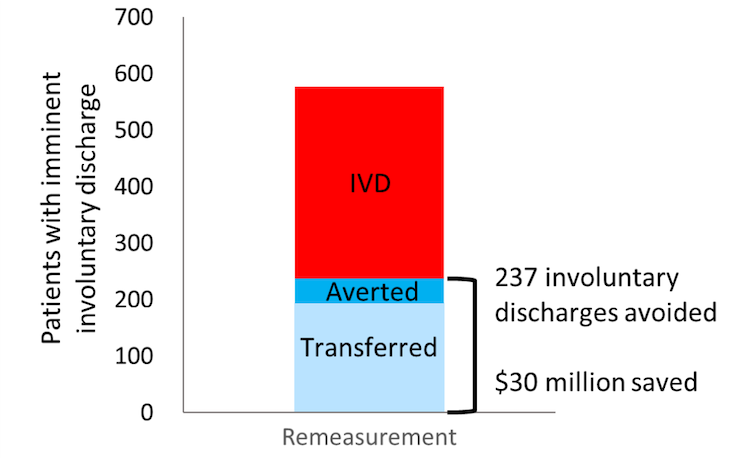
Of the 1,067 “access to care” cases in 2019, 237 patients were at risk of IVD with a 30-day letter. The Network helped to avert the IVD for 25 patients and helped the other 212 transfer another clinic. A single patient could have multiple types of access to care events. We don't know from that report how many patients were denied care or had a “failure to place” who may be getting emergency dialysis in hospitals.
Where are the data for patients treated at a clinic who were hospitalized for more than 30-days and then discharged from the clinic due to how CMS collects data? Some of those patients have been refused clinic readmission. For example, some patients who recovered from COVID-19 may have a trach now. I don't believe those patients are counted as IVD. Patients with trachs may be dialyzed in nursing homes and those with vents may get dialysis in hospitals, both of which cost Medicare more.
The High Cost of IVD
Taxpayers pay a high cost for care outside an outpatient dialysis clinic. The End Stage Renal Disease (ESRD) Network Program 2018 Summary Annual Report said there were 577 patients at-risk for IVD who received 30-day letters. That year, Networks helped avert IVD allowing patients to stay in their clinic or facilitated a transfer to another clinic for 237 patients. The per patient per year cost difference between outpatient dialysis and emergency dialysis in a hospital was $253,800. Avoiding IVD saved $30 million that year. If my math serves me correctly, there were still 340 patients who received 30-day letters where the IVD was not avoided, plus an unknown number of patients who had an expedited discharge for credible threats. I presume all those patients either dialyzed emergently in hospitals or died. Avoiding IVD in more of these patients would have saved even more.
Policy Changes Might Help
With so much money on the table, might CMS dig deeper into cases of IVD? ESRD Networks collect data on a lengthy list of reasons a clinic might report from non-compliance to inability to meet a patient's medical needs to barriers to access to care and failure to place. Giving clinics the option to report these reasons implies that they are allowed under the ESRD regulations, but are they? Are there any that could violate federal laws? I believe that greater data transparency on IVD/IVT is warranted at minimum for research and policy discussions.
CMS provides patient level adjusters to clinic reimbursement under the ESRD Prospective Payment System.
With more research on these data, might CMS add adjusters for some of the more commonly used reasons for IVD/IVT?
Might CMS consider including IVD/IVT as a reporting measure in the ESRD Quality Incentive Program (QIP)? With around 1,000 patients reported as having barriers to “access to care” in 2019, few patients experienced IVD/IVT, so if a clinic has had more than one episode in a year, there might need to be consequences, especially when interventions may be used to address why. To gain increased payment for more patients with considered comorbidities and/or avoid cuts because of too many IVD/IVT cases in a year, clinics might do a better job with acuity-based staffing for all disciplines taking those reasons into consideration. With better staffing:
Nurses and technicians might have more time to spend talking with patients to learn about their lives outside of dialysis and the challenges they face. This might help them to be less judgmental and punitive when patients do not follow their treatment plans 100%. It might give them time to refer patients to the social worker for mental health counseling and to address problems related to social determinants of health (SDOH).
Nurses and/or social workers might have time to teach staff how to work more effectively with upset people and those with pre-existing mental health diagnoses using the Decreasing Dialysis Patient-Provider Conflict manual that has tools and 8 group sessions and activities.
Administrators might provide social workers more support and time to address SDOH barriers to treatment and to counsel patients with anxiety and depression to help them manage their emotions, cope better with dialysis, and work more collaboratively with the healthcare team. In addition to helping to avoid IVD, this extra support for patients might reduce deaths and hospitalizations that cut into dialysis facility revenue.
Others' Views of IVD

A 2017 doctor's blog Involuntary Discharge for Dialysis: A Health Care Practice Like No Other says “Involuntary discharge from dialysis—a life-sustaining treatment — is a uniquely American phenomenon. It is not reported with any frequency in other first-world countries. In Canada, as just one example, it would be impossible to involuntarily discharge a dialysis patient from a treatment center.” In 2020, Involuntary Discharge from Dialysis: Has This Happened to You? addresses IVD from a number of angles. A nurse and technician interview a nocturnal home HD patient who describes herself as having been a patient advocate for 20 years with her Network and other national organizations. This blog and webinar give a bigger picture of IVD than data can provide.
Conclusion
IVD may not happen to many patients, but when it does, it is highly stressful and potentially deadly. Data present numbers, but do not show the full picture of the sequence of events leading up to a patient being at risk of or experiencing IVD. There are some extreme cases where IVD may be the only way to protect the safety and security of the clinic and its patients. However, as the dialysis regulations state, IVD should be rare. Are IVD cases rare enough? Is there more we could do as a community to reduce the number of IVDs to save patients' lives and taxpayers dollars? Only time will tell if the renal community and CMS have the will do that.


Comments
kim
Jul 23, 2022 6:27 PM
Crystal
Nov 03, 2023 2:20 AM
Amy Staples
Apr 14, 2022 10:01 PM