Pregnancy and CKD: Making it Possible, and the Legacy of Dr. Susan Hou

By Alicja Rydzewska-Rosołowska @alunieczka, AJKDBlog Guest Contributor. Blog post reproduced with permission from AJKD Blog
It took a strong woman to pioneer research in the field of women 's health and certainly Dr Susan Hou was one. During her career, she worked tirelessly to help us understand chronic kidney disease (CKD) and pregnancy; let 's not forget those were the times when “Children of women with renal disease used to be born dangerously or not at all – not at all if their doctors had their way.” Nowadays, although many unanswered questions remain, we have much more knowledge to guide us through the counseling and care of women with CKD who desire to become mothers, as reviewed by Oliverio et al.
To start, acknowledging the sexual and reproductive health of women with CKD has been identified as a patient priority. Sexual dysfunction is reported by 30%-80%. Many factors contribute: decreased arousal, increased pain, and greater sexual distress. Changes of the hypothalamic-pituitary-ovarian axis (summarized below) affect the fertility of women with CKD.
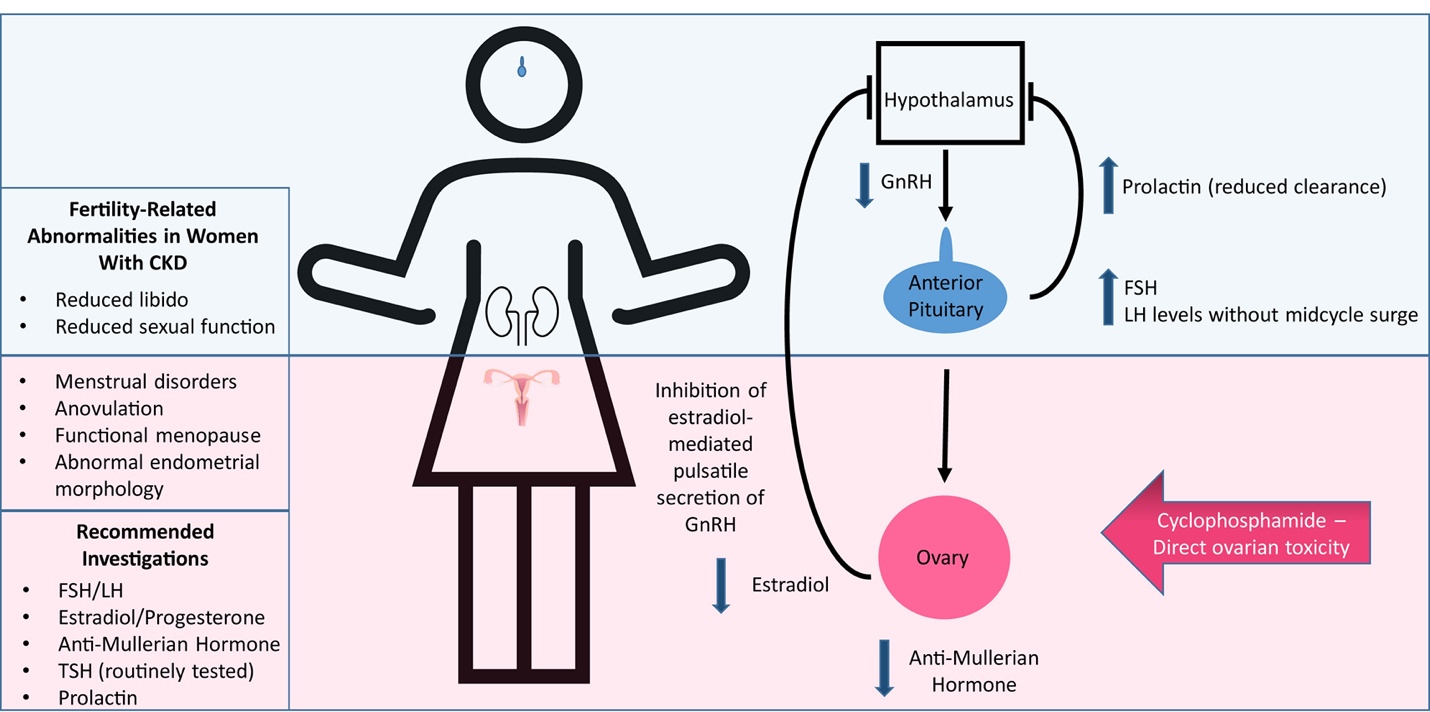
Figure 1 from Oliverio et al, AJKD © National Kidney Foundation
Fertility also diminishes as kidney disease advances. The available treatment is kidney transplantation, though longer dialysis sessions (nocturnal dialysis) may be another option. Medications like cyclophosphamide can cause ovarian failure in women requiring immunosuppression. In women with lupus, gonadotropin hormone-releasing analogues (leuprolide) decrease the frequency of persistent amenorrhea when co-administered with cyclophosphamide. Additionally, in vitro fertilization is feasible in women with CKD and, combined with preimplantation genetic diagnosis, may be an option for single-gene disorders such as autosomal-dominant polycystic kidney disease. Multidisciplinary pre-pregnancy counseling by both nephrologists and obstetricians helps women make informed decisions, improves potential outcomes and need to be accessible to all patients.
Maternal and fetal outcomes of pregnancy in CKD
The risk of adverse outcomes such as preterm delivery, lower birth weight, and decline in maternal kidney function rises at more advanced CKD stages, as does the need for higher-level neonatal care.
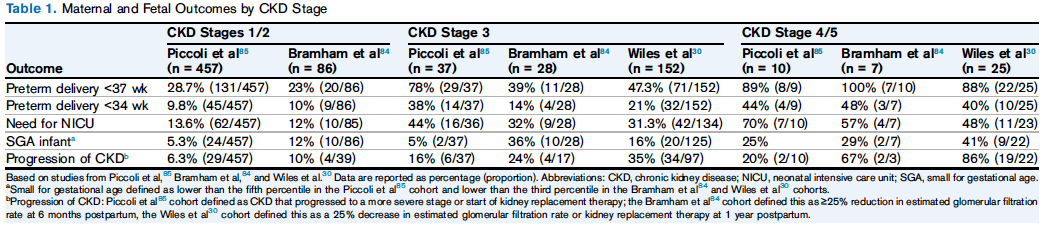
Table 1 from Oliverio et al, AJKD © National Kidney Foundation
Additional pregnancy-related complications may be present in women with lupus nephritis, and at least 6 months of stable remission is recommended prior to conception. In the PROMISSE study a severe postpartum flare occurred in only 1.7% of women with urinary protein-creatinine ratio <1 g/g and serum creatinine <1.2 mg/dl. Other glomerular diseases are less well studied and risk stratification should be individualized.
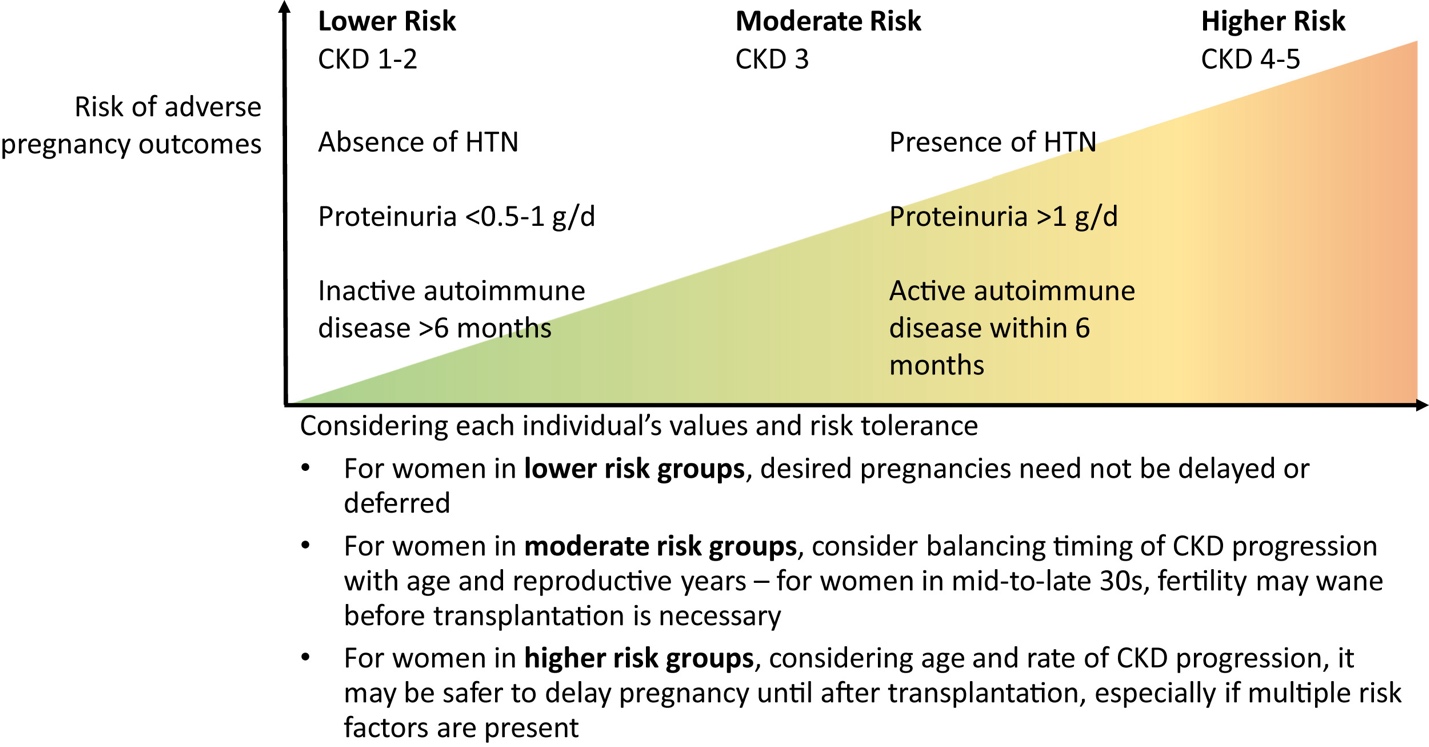
Figure 2 from Oliverio et al, AJKD © National Kidney Foundation
Preconception management
Certain modifiable risk factors can be addressed before pregnancy. Obesity increases the risk of miscarriage, gestational diabetes, preeclampsia, and cesarean delivery. Optimization of blood pressure control and medications used is also important. Recent data suggest that ACE-inhibitors do not increase the risk of major fetal malformations during the first trimester. The table below presents the fetal risk of common medications.
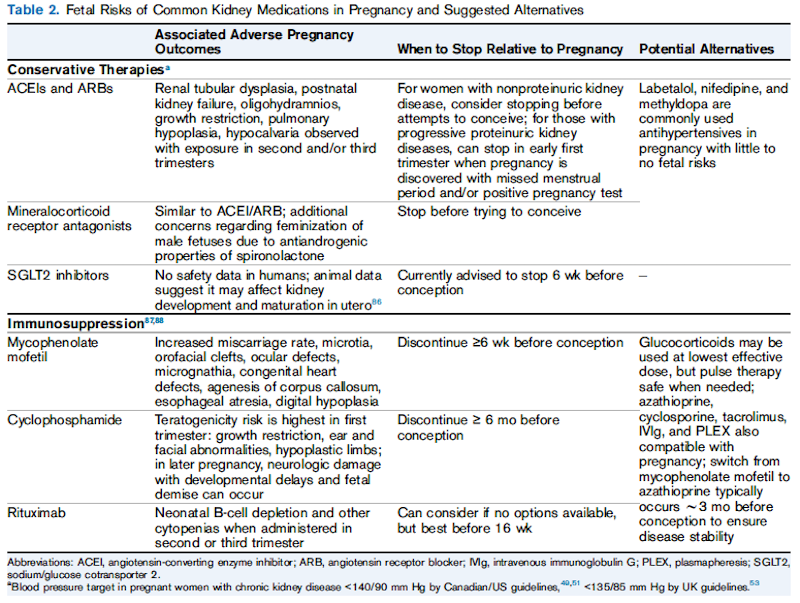
Table 2 from Oliverio et al, AJKD © National Kidney Foundation
In women with lupus, anti-Ro and anti-La antibodies are necessary due to the risk of congenital heart block. Hydroxychloroquine is advised for all pregnancies of patients with lupus, and checking anti-Ro and anti-La antibodies is important to determine the risk for congenital heart block. Blood pressure management should be monitored more frequently as the pregnancy proceeds, and treatment should be initiated at ³140/90 mm Hg based on the Canadian and UK guidelines.
Preeclampsia
Preeclampsia is new-onset hypertension with systolic blood pressure >140 mm Hg or diastolic BP≥90 mm Hg after 20 weeks ' gestation, together with one or more symptoms of maternal organ dysfunction and fetal growth restriction. Soluble fms-like tyrosine kinase-1 (sFlt-1) levels which antagonize angiogenic placental growth factor (PlGF) and vascular endothelial growth factor (VEGF) are higher in women with preeclampsia. In some studies of women without CKD sFLT:PlGF ratio or PlGF levels helped guide management (especially as a test to rule-out preeclampsia). Aspirin (75-150 mg/day) from the beginning of pregnancy is recommended for all women with CKD as it significantly decreases the risk of preeclampsia. When severe features of preeclampsia are absent expectant management is feasible up to 37 weeks of gestation.
Immunosuppression in pregnancy
Diagnosis of disease flare relies mainly on symptoms and serologic markers, although biopsy is feasible up to 30 weeks of gestational age (complication rate of 7% versus 1% within 2 months postpartum). Immunosuppression for various nephritis flares usually includes steroids, azathioprine, and/or calcineurin inhibitors. Rituximab can be used up to 16 weeks of gestational age (when immunoglobulin G transfer from mother to fetus begins).
Kidney replacement therapy in pregnancy
For patients that require dialysis and express a desire for pregnancy, observational studies have shown that intensifying hemodialysis improves live birth rates, gestational age, and birth weight. Women without residual kidney function should receive at least 36 hours of hemodialysis weekly, aiming for a midweek serum urea nitrogen level <35 mg/dl. Other recommended alterations are presented in the table below.
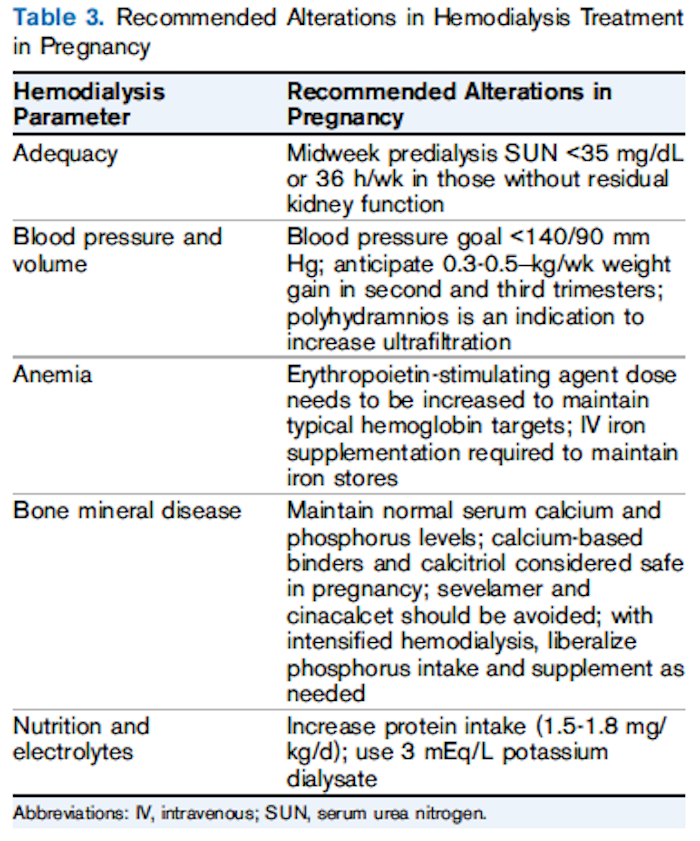
Table 3 from Oliverio et al, AJKD © National Kidney Foundation
Given worse pregnancy outcomes among women on peritoneal dialysis, a switch to hemodialysis before conception or early during pregnancy is recommended. Dialysis should be initiated for typical reasons, or when there is polyhydramnios, or serum urea nitrogen level reaches 45-50 mg/dl. For patients who receive a kidney transplant, conception can be encouraged 12 months after transplant surgery (if there are no rejection episodes). Mycophenolate mofetil should be withdrawn at least 6 weeks (and optimally 3 months) before pregnancy. Patients may need higher doses of calcineurin inhibitors. The live birth rate is 72.9% and incidence of graft loss within 2 years is 9.4%.
We have witnessed an unparalleled improvement in the care of pregnant CKD patients over the past 40 years; the rate of live birth among those undergoing dialysis increased from 22.9% in 1980 to 85%-90% in 2020. Future work should focus on individual risk-assessment for CKD patients desiring to become pregnant and optimization of the health and well-being of mothers with CKD and their children. Thanks to Dr Susan Hou, pregnancy on dialysis is no longer perceived as mission impossible.


Comments