Fostering Interdisciplinary Team Collaboration to Support Home Dialysis Patients


Our kidney care model works to address complex patient needs across dispersed geographies. Social workers with mixed modality caseloads may experience tensions which could result in less time spent with home patients. In our experience, home RNs generally have more in-person touch points with home patients as compared to other care team members. To help improve psychosocial support of home patients, and prevent the number of patients removed from home modalities due to psychosocial reasons, it is imperative for home social workers and home RNs to work closely together to bridge the gap of fewer contacts by the social worker.
We believe team training, strong processes and proper tools can strengthen communication, collaboration, and coordination of psychosocial care for Home patients.
Current State
Social workers often cover multiple facilities and multiple modalities. Home RNs may cover one or two modalities, and more than one facility. Both the social worker and home RN are responsible for evaluating the patient’s home environment. Covering multiple facilities and multiple modalities has its challenges, including driving time, access to medical records, coordination of schedules, modality specific needs, geographic specific needs, and urgent clinic visits:

Driving Time: Social workers and RNs must allocate time for commuting, which could otherwise be spent on patient care responsibilities.
Access to Medical Records: Electronic Health Records (EHRs) have helped – however paper medical records and fax machines are still a part of daily life.
Coordination of schedules: One of the biggest challenges is aligning schedules for the patient, physician, nurse, social worker, and dietitian. It can be difficult to bring the entire care team together at the same time on a regular basis.
Modality-specific Needs: Social workers and Home RNs should be skilled at assessing and supporting the unique challenges home patients are faced with. Home patients may experience challenges with setting up treatments, cognitive impairment, fear and anxiety about their inability to perform treatment, depression, and heightened levels of burden due to reliance on family members and limitations of space or a clean home environment. If not addressed by the care team, these challenges may be a contributing factor(s) to patients leaving their modality of choice.
Geographic-specific Needs: Our experience is that patients who live in urban settings may experience differential challenges compared to patients who live in rural areas. Home social workers and home RNs should be skilled at assessing and supporting patients regardless of their geographical location. Patients living in an urban area may be more likely to experience home space limitations for supply storage, language barriers, and homelessness. Patients in rural areas may also be faced with similar challenges, however, when these challenges are experienced in a rural area, often times resources are more limited than in large metropolitan areas, and can be more challenging to navigate.

It is important for both the social worker and nurse to collaborate, communicate, and coordinate responsibilities to be an efficient team. The logistics of coordinating home weekly Interdisciplinary team (IDT) meetings, plan of care meetings, quality assurance meetings, rounding schedules, lab draws, physicians’ schedules, and staff training can be extremely challenging. The entire team must possess a high level of collaboration and communication to help ensure everyone is on the same page.
Communication and Collaboration Methods
In January 2022, we polled 24 Home RNs and 60 Home social workers with the question, “What is your primary method of communication with the ‘Home MSW’ and ‘Home RN’?” respectively. For home RNs, the top two responses were email and other. For Home social workers, the top two were other and Clinic Day. The least chosen response from both groups was “Regularly Scheduled Meetings.” Interestingly enough, we asked the same group “How effective are weekly core team meetings regarding meeting the psychosocial needs of home patients?” 78% responded in the effective range of the 5-point scale. We feel the regular meetings play a crucial role in strengthening communication, collaboration, and coordination of psychosocial support of home patients. A team in oncology has noted, “When health care professionals are able to efficiently and effectively communicate, consult, and generate discipline - and team - specific care plans, patients benefit.”1
Goltz and colleagues noted that when it came to RNs and social workers, “We were unable to locate other models or standards of care that facilitate interdisciplinary collaboration and cooperation between these essential disciplines.”
Standard of Care

CMS defines the IDT as consisting of, at minimum, “the patient or the patient's designee (if the patient chooses), a registered nurse, a physician treating the patient for ESRD, a social worker, and a dietitian.” The CMS ESRD Interpretive Guidance states, “Interdisciplinary teams work collaboratively with regular meetings to discuss patient status and the evolving plan of care. Working as a team allows for working toward common goals, pooling of expertise, and a forum for problem solving“(V501; emphasis added). If regular IDT meetings are a standard imposed by CMS, why were Goltz and colleagues unable to find other standards and models of care outside of oncology? Our opinion is the standard of care exists today, but can and should be refined with training/process/tools to elevate the current state of communication, collaboration, and coordination of care. This begins with the prioritization of regularly scheduled IDT meetings.
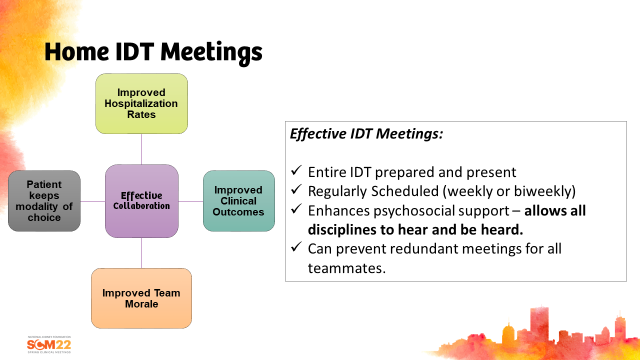
Fig 1
As a team we strive to support our patients to remain on their modality of choice. As you can see in Fig 2 below, many of our PD patient losses occur between 1-2 years on therapy; 55% of modality losses occur after the first year. Why is this? The two main drivers of patient modality loss are infection and psychosocial factors (these two often contribute to one another). How do we change the trajectory? We believe home patients require more support from the IDT to prevent therapy exhaustion and complacency. It’s also important to note the timing of when support is needed and when risk factors are identified. It’s critically important for teams to meet regularly to discuss patients holistically. Important discussion items are: plans for assessments and evaluations at IDT determined time on therapy, developing team care plans for identified challenges, discussing process of care plans, working together to resolve any barriers preventing success, and collaborating on home environment evaluations.
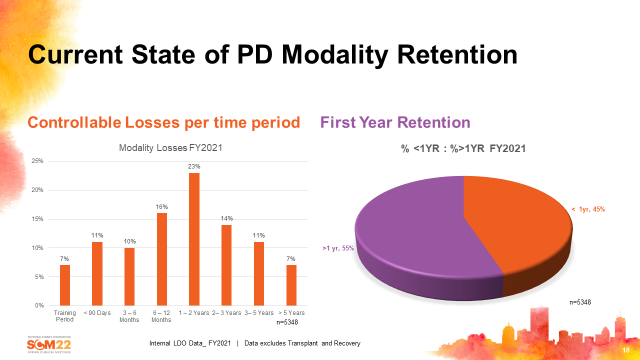
Fig 2
As noted in an observation of ~1300 facilities between Jan and March, 2020, and ~1300 facilities between April and June, 2020 (Fig 3), teams who engage in more frequent IDT meetings have notably lower controllable PD loss rates (excludes transplant, death, incarceration, move to another facility on PD) compared to teams that do not meet frequently. It’s not always easy to get everyone together at the same time each week, but this evidence suggests it can be very important to address the causes of modality loss. It requires outstanding coordination and flexibility of schedules, and excellent communication with the entire team.
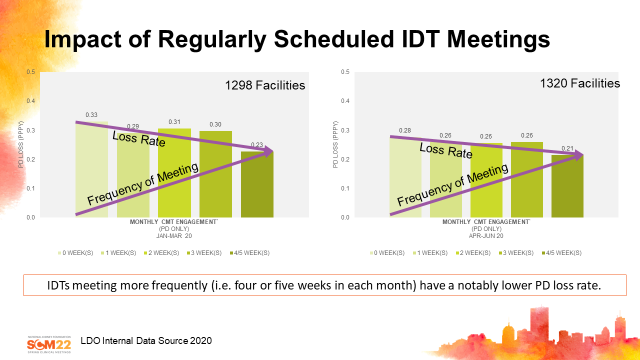
Fig 3
Using the Data to Plan for Success
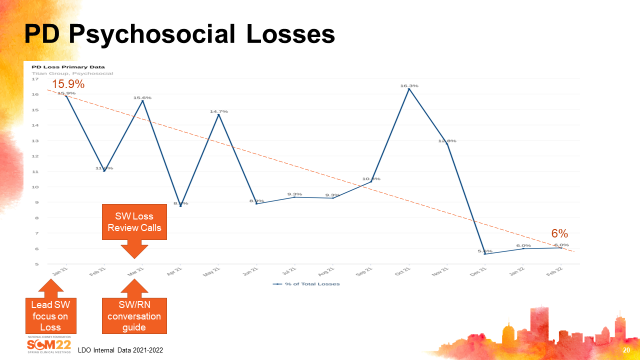
We identified that psychosocial losses were our top reason for non-modality loss in 2021. Based on these data, we increased our awareness and focused on psychosocial losses. Lead social workers started monitoring and reporting their psychosocial losses to senior leadership on a monthly basis. We implemented monthly calls with PD social workers to review losses. We implemented a SW/RN partnership guide that mapped out the roles and responsibilities of the PD RN and PD social worker. We also encouraged IDT teams to meet weekly and categorize their PD modality losses together to ensure losses were categorized correctly, resulting in increased confidence in our loss data.
In addition to the processes put in place to increase awareness, collaboration and communication, social workers administered the Distress Thermometer (DT) to identify patients experiencing elevated levels of distress. Based on the patient’s DT score, the appropriate discipline targeted the area of distress to help patients and/or their care partners resolve the area of concern.
Social workers also administered a PHQ-9 depression screening tool to identify patients experiencing depression. The PHQ-9 helps the IDT understand and have sensitivity to the mental and emotional challenges patients are experiencing that can impact treatment adherence. Patients experiencing depression were engaged in more frequent contacts by the PD social worker to provide additional psychosocial support.
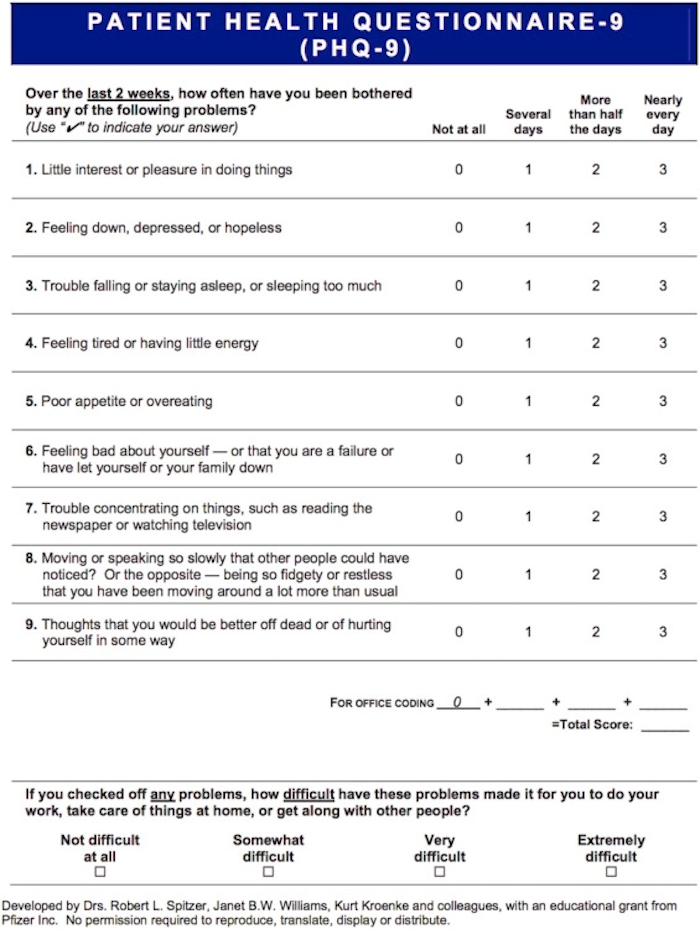
These tools were essential in helping the team identify patients who could benefit from increased contacts and psychosocial support. Based on an internal analysis of patients (in-center hemodialysis (ICHD and Home), patients who received additional psychosocial support had a 52% reduction in DT score, and a 42% reduction for patients with 10+ PHQ-9 score.
This demonstrates how using these tools can make a measurable and meaningful difference in the care social workers are able to provide patients, and how the entire IDT can come together to provide a holistic approach to patient care. Sharing DT scores with IDT members allows the team to be very strategic in their approach in terms of who is going to target the specific areas of distress, whether its physical distress addressed by the physician, RN, or outside referral, or supportive counseling by the social worker to target emotional, social, and spiritual concerns. Likewise with PHQ-9 scores. The home social worker and home RN communicating about specific interventions, referrals to community resources, and coordinating medication management with the PCP and/or mental health professionals, allows everyone to work together to enhance the psychosocial support given to home patients who are experiencing distress and depression.
Shared Electronic Calendar

Another process we encouraged teams to adopt is utilizing a shared electronic calendar. Coordinating schedules, especially when IDT members travel to multiple clinics, is challenging, but achievable. Physician clinic days are often scheduled months in advance. Dietitians and social workers usually have set days they are in their clinics and can communicate this to the person coordinating the calendar. It requires commitment by everyone to coordinate their schedules to make IDT meetings a priority, and ideally attend in-person, and if not in-person then by phone or video call.
The pandemic has made many aspects of patient care more challenging, especially if there are staffing challenges and limited coverage options. In situations where there are staffing challenges, it may not be possible to meet every week and coordinating schedules and calendars is more complex.
We recommend teams commit to ensuring they are consistently meeting with one another, ideally on a weekly basis, to communicate and coordinate care as a full IDT. Based on our experience, PD patients tend to have lower loss rates if the care team meets weekly. We encourage prioritizing core team meetings, and planning your day around core team meetings, rather than planning core team meetings around your day. When staffing is a challenge, adjustments likely need to be made.
Home Visits

RNs and social workers who visit patients’ homes during initial onboarding, when challenges are identified (i.e. peritonitis episodes), and on an annual basis, could reduce psychosocial risk factors that lead to patients switching off their modality of choice. We reviewed modality conversion data for a small data set of 21 home social workers who stated they consistently visited the patients’ home during initial onboarding. The result was ~15% reduction in PD to ICHD modality conversion in the social worker cohort that consistently visited patients’ homes.
We recognize more data are needed in this area, but hope to see more teams consider the importance of collaborative home visits. Social workers may request training and support to gain comfort with home evaluations.
To summarize, improving communication, collaboration, and coordination between Home social workers and Home RNs can be achieved with frequent regularly scheduled meetings (we encourage a shared electronic calendar). Other recommended practices include mapping out the responsibilities of each team member, adopting tools like the DT and PHQ-9, being prepared to discuss key focus patients, developing team specific plans, and considering collaborative home visits as a team responsibility.
Goltz HH, Major JE, Goffney J, Dunn MW, Latini D. Collaboration between oncology social workers and nurses: a patient-centered interdisciplinary model of bladder cancer care. Semin Oncol Nurs. 2021 Feb;37(1):15114↩︎


Comments