Understanding & Explaining Dialysis Charges & Payment

Have you ever had a patient ask you ”How does Medicare (or insurance) cover and pay for dialysis?” Here’s how you can answer that question.
Medicare Coverage and Payment
Medicare covers in-center dialysis and home dialysis under Part B. Original Medicare’s allowed rate per dialysis treatment is the same for those with permanent kidney failure (ESRD) or acute kidney injury (AKI). Original Medicare’s payment for dialysis is bundled and includes ESRD-related labs and drugs. Payment for home dialysis includes a machine and supplies as well as support equipment such as:
A scale (for a wheelchair if the patient can’t stand)
Manual BP monitor
Basic adjustable chair for hemodialysis (HD) done during waking hours
Medicare reimburses for three hemodialysis treatments a week unless the doctor writes a letter of medical justification for more. It pays the same amount per week for three HD treatments and seven days of peritoneal dialysis (PD). Medicare now lets dialysis clinics treat patients with AKI and can treat them and bill for as many treatments per week as the doctor prescribes.
Home dialysis training and treatments are covered for people with ESRD—but not AKI. A home dialysis helper is not covered. Dialysis providers are lobbying to get Medicare to cover home dialysis training and home dialysis for people with AKI. (CMS is concerned that those with AKI often need closer monitoring. because they can have more complications.)
The ESRD Prospective Payment Rate
The ESRD bundled rate is called the prospective payment system” (PPS). CMS increases the ESRD PPS rate each year. In 2022, the base rate is $257.90 per treatment, with some adjustments. If you want to learn more about the ESRD PPS details, read this CMS fact sheet.
The proposed base ESRD PPS for 2023 is $264.09, an amount that could change in the final rule. Again, there some adjustments. Here’s a fact sheet about the proposed PPS rule.
Dialysis Clinic Charges to Commercial Payers
Dialysis clinics can charge commercial insurers much more than what Medicare allows as “reasonable and customary.” How much any insurer pays depends on the contract it has with the dialysis provider—if it has one at all. Patients on Home Dialysis Central’s Facebook group have reported receiving insurance explanations of benefits (EOBs) showing dialysis bills of $100,000 or more PER MONTH. The insurance company may pay a lot less than what the clinic bills. However, how much any patient must pay of these bills depends on how their policy is written and whether the provider is or is not a preferred in-network provider. Some dialysis providers will discount bills for patients who meet their guidelines—if they share very personal financial information.
Medicare as a Secondary Payer
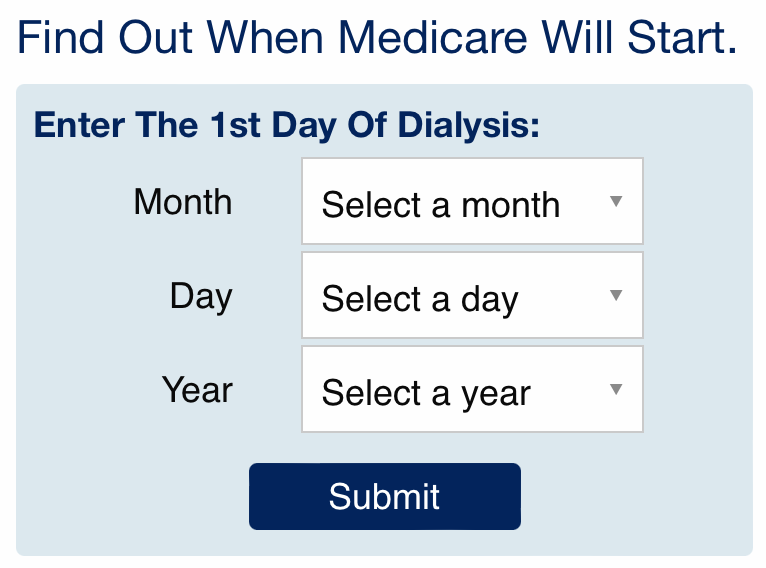
When a dialysis patient has a job-based plan, that plan pays first for 33 months if the new patient chooses in-center dialysis or 30 months if the patient starts home training during the 3-month Medicare qualifying period. This calculator will help you—and your patients—see when Medicare will start to pay, depending on which treatment option they choose.
Some patients ask why they should enroll in Medicare and pay the Part B premium if they have a job-based plan. They need to understand that having Medicare as a secondary payer during those 30- or 33- months will limit what dialysis providers can charge them. Let’s say an insurance plan has an annual deductible and copays/coinsurance for clinic visits. When a dialysis provider bills a commercial payer more than Medicare allows, but the plan pays at least 100% of Medicare’s allowed charge (most do), the dialysis provider cannot bill the Medicare patient anything under “assignment of benefits” rules.
Medicare as a Primary Payer

When Medicare is a patient’s primary payer, how much the patient could owe of Medicare’s deductible and coinsurance depends on how their other insurance plan coordinates with Medicare. Medigap plans pay most or all of the Part B 20% coinsurance. Some job-based plans do, too. But others “carve out” Medicare payment and limit what they pay. For the 30-month Medicare secondary payer period, the plan will pay a huge amount for their member’s dialysis.
Help for Medicare Premiums

Dialysis patients with limited income and assets may get help to pay their premiums from their state if they have Medicaid or a Medicare Savings Program. Dialysis providers donate to the American Kidney Fund, which helps pay eligible patients’ insurance premiums through its Health Insurance Premium Program (HIPP). The two largest donors to the AKF’s HIPP are DaVita and Fresenius. These companies treat most of the U.S. dialysis patients. When a donation goes to paying commercial insurance premiums, according to this article, dialysis providers get a return on investment (ROI) of $3.50 for each $1 donated. They get much less ROI for their donations when a patient has a Medigap plan with Medicare that covers only 100% of Medicare’s allowed charge.
Clinic Responsibilities
Dialysis costs a lot. Most dialysis patients qualify for Medicare, but some don’t take it. Financial concerns can contribute to stress, difficulty following the treatment plan, and behavior issues. The ESRD regulations at 42 CFR 494.70(a)(11) require dialysis clinics to inform patients about charges that are not covered by Medicare. These regulations do not explicitly require clinics to inform patients about what they could owe when Medicare covers dialysis and related care or with their other insurance. That said, it seems only reasonable for dialysis billing staff to verify insurance and help a patient understand what is and is not covered and what they might owe. Dialysis financial counselors or clinic social workers should refer patients to resources for financial help for which they may qualify. Doing anything less is short-changing patients.


Comments
Beth Witten
Sep 17, 2023 11:28 PM
If you run a transportation business, I'd suggest you contact your state Medicaid office and see what you would need to do to become a Medicaid transportation provider, how to bill for dialysis-related trips (which are called non-emergency medical transportation and are Medicaid covered), and what the reimbursement would be. You could also find out if your county has paratransit services for elderly and disabled people and what it would take to provide transportation under that agency. Before there was Uber or Lyft, I had taxi drivers who regularly drove my patients. It worked well for my patients and the drivers as well.
Timothy Lofton
Aug 01, 2023 10:10 AM