Advance Care Planning, End of Life Decisions, & Religious Views on Stopping Dialysis

Background
Patients who do home or in-center dialysis may have a single condition that caused their kidney failure, or may have multiple conditions. Those conditions may be manageable with diet, exercise, medications, and other treatments. But, sometimes people have pain and are so debilitated that their quality of life is poor, and they question whether life is worth living or if it’s time to consider stopping dialysis.
When a patient asks about or is considering stopping dialysis, the IDT should consider this patient unstable. The ESRD CfC requires unstable patients to have a full IDT reassessment and plan of care. In assessing the patient and planning care, consider:

Is the patient doing the type of dialysis that fits best with what is important to him/her? My Kidney Life Plan is a tool to help patients see if there’s a different type of dialysis that fits better. The IDT should help individuals get the type of dialysis that fits better, whether at the current clinic or elsewhere.
What does the KDQOL survey show? If a patient is talking about stopping dialysis, ask him or her to take the survey so you can see if there is anything new. Look beyond the scores to how the patient answered all the questions. Looking at the answers to the first 12 questions can tell you how s/he is doing physically and emotionally. Questions on the burden of kidney disease (13-16), symptoms/problems (17-28), and effects of dialysis on daily life (29 to 36) can give you ideas of actions to take to improve how someone feels.
Is the patient’s prescription or dialysis and medications allowing him/her to do what s/he wants/needs to do? Consider changes and discuss them with the patient to help him/her understand why you suggest them. Be aware that dialysis regulations allow patients to refuse.
What nutritional or psychosocial needs does the patient have that could be factors? Poor nutrition can affect energy and physical functioning and social health needs can contribute to depression and anxiety.
Has the patient been screened recently for depression and anxiety? The ESRD Quality Improvement Program requires dialysis clinics to screen most patients for depression.1 Patients can refuse to be screened. However, a patient may complete the survey after the social worker explains that depression increases the risk of hospitalization and death, and treatment can reduce those risks and improve quality of life. If screening showed a positive result, there are brief counseling tools that the social worker can use with the patient during dialysis. Using the tools in as little as 1.5 hours spread out over a six-week period was shown to reduce depression and improve health-related quality of life.2 If the social worker’s license and scope of practice does not allow him/her to do counseling or the social worker’s caseload may limit time to provide even brief counseling, s/he can refer the patient to a community mental health provider with experience working with people who have chronic illness. There are many potential barriers to a patient seeking outside counseling, including but not limited to lack of motivation, stigma associated with mental illness, more time away from home, transportation, few mental health providers in some areas that accept Medicare and/or insurance, and cost. A social worker who refers out should identify any barriers to accessing that help and work to resolve them.
Has the patient been offered a peer mentor? Patients can feel as if they’re the only one who knows what it’s like to have kidney failure and be on dialysis, which can cause a sense of isolation. Providing opportunities for peer support can help relieve that sense of aloneness. A randomized controlled trial found that dialysis and transplant patients who received a textbook about kidney disease and support from a trained peer using an online bulletin board at least monthly had significantly improved health-related quality of life.3 Several nonprofit organizations offer opportunities for telephone or online peer support including the Medical Education Institute’s Home Dialysis Central Forum bulletin board and Home Dialysis Central members only Facebook group, the National Kidney Foundation’s PEERS, and the Renal Support Network’s Hopeline. Dialysis clinics can train and use their own patients as mentors.


Advance Care Planning (ACP)
The Patient Self-Determinations Act (PSDA) of 1990 required hospitals, nursing homes, home health agencies/personal care services, hospice providers, and health maintenance organizations receiving Medicare or Medicaid funds to provide their patients information about advance directives.4 Dialysis clinics were not required to do this under this law. However, the 2008 ESRD Conditions for Coverage states at 42 CFR 494.70(a) that a patient has the right to “Be informed about his or her right to execute advance directives, and the facility's policy regarding advance directives.”5 The interpretive guidance says that if the clinic will not honor a patient’s advance directive(AD), the clinic should help the patient transfer to a clinic that will. ADs allow patients to state what treatments they would choose or refuse if they were unable to communicate their wishes. A durable power of attorney for healthcare decisions (DPOAHC) allows the patient or name someone they trust—family, friend, or even their doctor—to serve as their proxy to make healthcare decisions for them. Caring Info, a program of the National Hospice and Palliative Care Organization provides state-specific advance directive forms here. The site has multiple resources related to ACP.

Since 2016, Original Medicare has covered the ACP conversation with no deductible or coinsurance when that discussion takes place during the face-to-face annual wellness visit. If the ACP talk takes place during a treatment visit, as with the treatment visit itself, there is a deductible, and 20% coinsurance could be covered by a Medigap or other plan.6 Patients without Medicare who have other health plans would need to check their policy for coverage.
Preferably an ACP conversation took place long before this, but if a patient is talking about stopping dialysis, there should be a discussion of the care s/he would want. Because of his/her medical training and experience, the doctor is the best person to talk with the patient about his/her condition, prognosis, and symptoms to expect if stopping dialysis. The doctor and social worker can help the patient understand the POLST/MOLST/POST (physician order for life-sustaining treatment/medical order for life-sustaining treatment/physician order for scope of treatment) and offer hospice. The social worker can talk with the patient about how to talk with family and friends. An article answers these 4 questions related to social work practice and ACP:
When should ACP conversations be initiated?
Where should ACP conversations occur?
Who initiates ACP conversations?
What is ACP content?7

It suggests these psychosocial interventions:
Mindfulness meditations
Deep breathing exercises
Relaxation techniques
Problem-solving counseling
Assertive communication training
Family counseling
Worry management planning
Sleep hygiene exercises
Anticipatory grief support8
Dialysis Withdrawal & Data
Patients who choose to withdraw from dialysis may live days or weeks depending on how much residual kidney function s/he has and whether s/he limits high potassium foods that can affect muscles—including the heart. Although it can be a challenge for a dialysis patient to get admitted by a hospice agency, patients who choose to stop dialysis can access hospice services, which are Medicare-covered.9 Anxiety or discomfort the patient feels can be managed with medications and by limiting fluids to limit fluid overload and shortness of breath. Dialysis staff may want to share the booklet When Stopping Dialysis Treatment Is Your Choice: A Guide for Patients and Their Families when discussing this option with patients.
The United States Renal Data System tracks data on patients with chronic kidney disease, as well as those on dialysis and with transplants. The 2021 Annual Data Report Reference Table on mortality (Table H) shows that the unadjusted rates of withdrawal for both HD and PD patients in 2017-2019 was 25.9%. This percentage may reflect those who withdrew because they were expected to die imminently from another cause. Examining the demographics of those who withdrew, they were more likely to be 75 or older, Caucasian or Native American, and much less like to be any other age group or race or ethnic group.10
Religious Views on Stopping Dialysis11
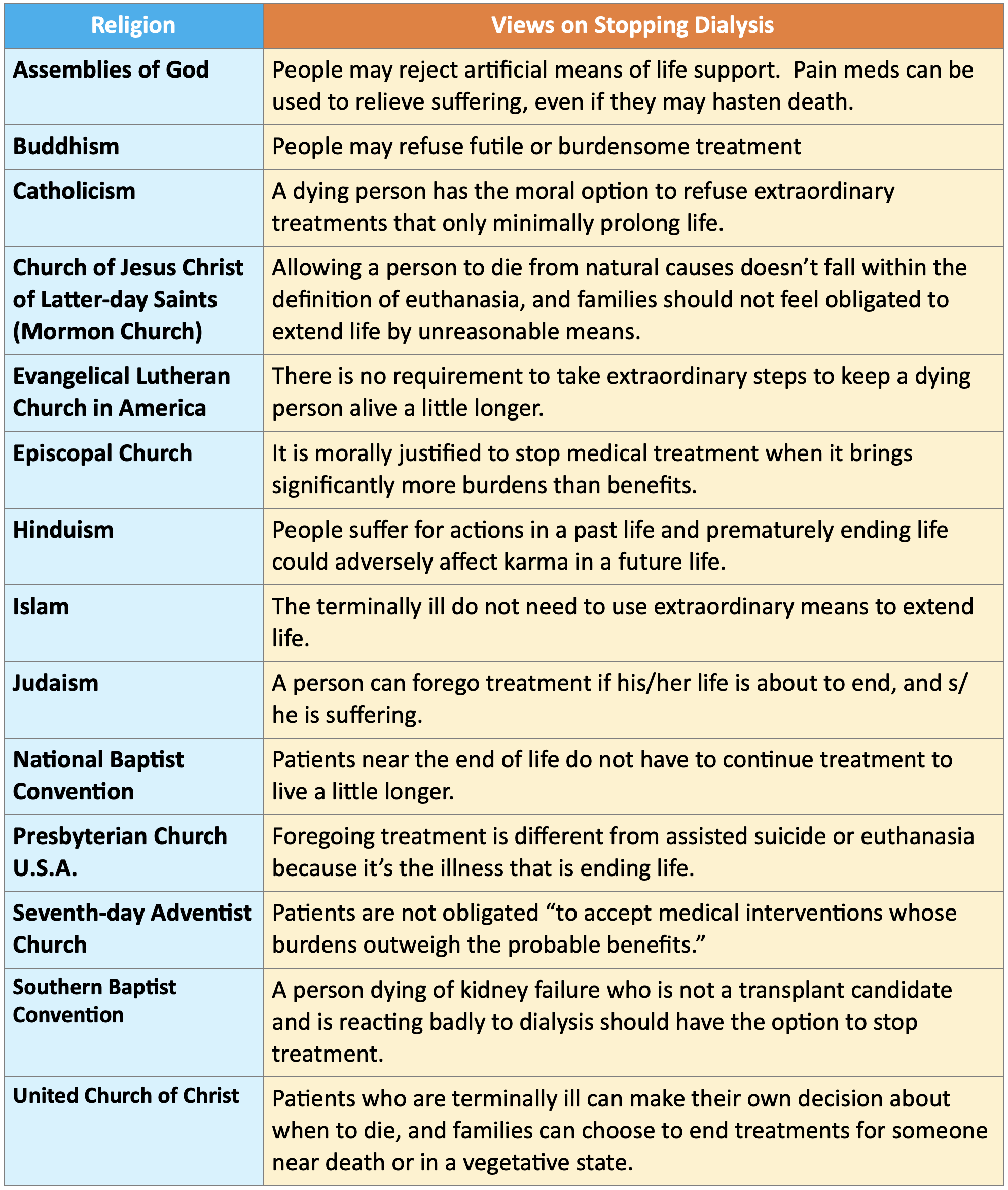
The Pew Research Center produced a report that describes various religions beliefs about end of life that addresses beliefs about physician assisted suicide, euthanasia, and whether it’s necessary to extend life with extraordinary means when terminally ill. The report includes links to references. As we all know, without dialysis or transplant, kidney failure will lead to natural death. The table below does not address physician assisted suicide or euthanasia, but focuses on whether it’s necessary to use extraordinary means to extend the life of someone who is terminally ill in the views of different religions.
Conclusion
Some people think of ACP discussions as morbid or sad. This may stem from our own feelings about and fears of death and dying. Dialysis staff may be uncomfortable with ACP discussions and may not realize that patients know dialysis is sustaining their life and they could die at any time. Knowing what they would choose or refuse gives our patients a chance to direct how they want to live and when they want to die if dialysis becomes too burdensome. Overcoming our discomfort enough to allow them to share their concerns and wishes is to honor them.
Centers for Medicare & Medicaid Services (CMS) End-Stage Renal Disease Quality Incentive Program (ESRD QIP) Calendar Year (CY) 2023 Measure Technical Specifications. Rule of Record: Calendar Year (CY) 2023 ESRD Prospective Payment System (PPS) Proposed Rule, July 8, 2022, pp. 32-33. https://www.cms.gov/files/document/cy-2023-proposed-technical-specifications-20220708.pdf-0↩︎
Sledge R, Aebel-Groesch K, McCool M, Johnstone S, Witten B, Contillo M, Hafner J. Part 2. The promise of symptom-targeted intervention to manage depression in dialysis patients: improving mood and quality of life outcomes. Nephrol News Issues. 2011 Jun;25(7):24-8, 30-1. PMID: 21736132. https://pubmed.ncbi.nlm.nih.gov/21736132/↩︎
Ghahramani N, Chinchilli VM, Kraschnewski JL, Lengerich EJ, Sciamanna CN. Effect of Peer Mentoring on Quality of Life among CKD Patients: Randomized Controlled Trial. Kidney Dis (Basel). 2021 Jul;7(4):323-333. doi: 10.1159/000514477. Epub 2021 Mar 31. PMID: 34395547; PMCID: PMC8314752. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8314752/pdf/kdd-0007-0323.pdf↩︎
PL 101-508, Sec. 4751, November 5, 1990. https://www.congress.gov/101/statute/STATUTE-104/STATUTE-104-Pg1388.pdf↩︎
Medicare and Medicaid Programs; Conditions for Coverage for End-Stage Renal Disease Facilities, April 15, 2008. https://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/Downloads/ESRDfinalrule0415.pdf↩︎
Medicare. Advance care planning. https://www.medicare.gov/coverage/advance-care-planning↩︎
Anderson EB, Waldrop D. Integrating advance care planning within the psychosocial care of nephrology patients. Jour Nephrol Soc Work. 2020. 44(1):13-17. https://www.kidney.org/sites/default/files/v44a_a2.pdf↩︎
Hunter CL., Goodie JL, Oordt MS, Dobmeyer A C (2009). Integrated behavioral health in primary care: Step-by-step guidance for assessment and intervention. Washington, D.C.: American Psychological Association.↩︎
Medicare. Hospice Care. https://www.medicare.gov/coverage/hospice-care↩︎
United States Renal Data System. 2021 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2021. Tables H.12_HE and H.12_PD.↩︎
Pew Research Center. Religious Groups’ Views on End-of-Life Issues. November 2013. https://www.pewresearch.org/religion/2013/11/21/religious-groups-views-on-end-of-life-issues/↩︎


Comments