Home Dialysis in the 2022 United States Renal Data System Annual Data report

Introduction to the USRDS ADR
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) provides funding to publish an annual data report (ADR) each fall. Data for the USRDS ADR come from Medicare (CMS), the United Network for Organ Sharing (UNOS), and the ESRD Networks and provides data on people with Original Medicare (Part A and B). The ADR consists of two volumes—one for data on chronic kidney disease (CKD) with eight chapters and the other on end stage renal disease (ESRD) with 12 chapters.

The 2022 ADR has two supplements—one on COVID and one on racial and ethnic disparities and the U.S. government’s Healthy People 2030 objectives for CKD. The website for the USRDS includes text and Excel reference tables that show even more granular data than the interactive text.
ADR Data on Home Dialysis
In 2021, the ADR devoted a chapter to home dialysis for the first time. In 2022 the ADR again provides data on peritoneal dialysis (PD) and home hemodialysis (HD). This blog will report some key things you might be interested in knowing about home dialysis in the U.S. as of 2020. NOTE: The data on home HD do not separate those doing dialysis in their private residence from those getting dialysis in a nursing home or other residential facility.
Small Changes in Home Dialysis Use

In 2020, the president issued an Executive Order called Advancing American Kidney Health Care that directed CMS to promote home dialysis and transplant. The CMS Center for Innovation designed End Stage Renal Disease Treatment Choices (ESRD ETC) model and required dialysis clinics in certain hospital referral regions to participate. The hope was that this model would spur growth in home dialysis by providing financial incentives for clinics that increased their percentage of home dialysis patients and reimbursement cuts for clinics that didn’t. When this took effect in 2021, home dialysis utilization was lower in clinics assigned to participate in this model. By Q1 2022, ETC clinics had 15% of their patients on home dialysis—compared to 14% in non-ETC clinics. Overall, the percent of incident patients on home dialysis grew from 6.8% in 2010 to 13.3% in 2020, while the percent of prevalent patients on home dialysis grew from 9.1% in 2010 to 13.7% in 2020.
Where Home Dialysis was Offered in 2020
There were 8,088 Medicare certified dialysis clinics in 2020. Almost half (45.6%) were not certified to do peritoneal dialysis (PD) or home HD, and 10% of the clinics certified for home dialysis had no active patients at the end of 2020. So, only 44.4% of the clinics certified for PD or home HD in 2020 had any patients on either treatment. More than 50% of PD programs and almost 87% of home HD programs had ten or fewer patients. The ADR did not report outcomes by clinic size, but hypothesized that size might impact outcomes.
Who Had Access to Home Dialysis in 2020

Age seemed to affect access to home dialysis. The highest percentage of patients on PD and home HD were ages 18-44 and the lowest were 75 or older.
A similar percentage of males and females were on PD, but more males than females were on home HD.
Race also seemed to matter. The highest percentage of PD patients were Asian, and the lowest were Black. The highest percentage of home HD patients were White and lowest were Hispanic and Asian.
Employment was higher in incident patients on PD (25%) and home HD (21%) than in-center HD (9.9%).
Insurance status seemed to impact which incident patients did home dialysis.
Medicare as a secondary payer was much more common among patients on PD (12%) and home HD (11%) than in-center HD (less than 4%).
Those with Medicare and Medicaid were more likely to do in-center HD (9.4%) than PD (7%) or home HD (8.3%).
Those with Medicare Advantage plans were more likely to do in-center HD (28.5%) than PD (22.8%) or HOME HD (22.4%).
Those with “other” insurance were more likely to do in-center HD (38.4%) compared with PD (30.5%) or HOME HD (32.8%).
Incident and prevalent patients living in poorer neighborhoods according to the Social Deprivation Index were more likely to be on in-center HD than PD or home HD.
In both incident and prevalent patients, those living in rural areas were slightly more likely to be doing PD or home HD than those in urban areas.
The primary cause of kidney failure seemed to affect access to PD and home HD. The lowest percentage of patients on PD or home HD had diabetes or hypertension.
Timing of Home Dialysis Starts
More than 86% of patients started PD in their first year of dialysis. Fewer patients (42%) on home HD started during their first year, and 20% started after 5 or more years on dialysis.
Length of Home Dialysis Training
Medicare covers up to 15 training days for PD. Almost 39% of PD patients were trained in 7-9 days—the most common length of PD training in 2019, and, 62% were still on PD in 2020. However, 11% were trained for PD in just 1-3 days in 2019—and, by 2020, 21.5% had died and 22.9% were on in-center HD.
Medicare covers up to 25 training days for home HD. Almost 27% of home HD patients were trained in 16-20 days—the most common training length for home HD—and 55% were still on home HD a year later. However, 12% of home HD patients received just 1-5 days of training in 2019. By 2020 almost 19% had died and 40% were on in-center HD.
PD Cycler Use
The percentage of patients using a PD cycler increased from 69% to more than 86% between 2010 and 2020. In 2020, patients 75 and older were less likely to be using a cycler than those 18-44. Slightly more males than females used a cycler and slightly more Black patients than White or Hispanic patients. Fewer Asian patients and patients of other races were using a cycler than Black patients.
Number of Home HD Sessions Prescribed Per Week
In 2020, 91.5% of patients ages 18-44 were prescribed 4 or more home HD treatments a week vs. 41.9% of those 75 or older. Only 10% of patients ages 18-44 were prescribed 3 or fewer treatments compared with 25% of patients 75 or older. More males (88%) were prescribed 4 or more treatments a week than females (84.1%). There was not much racial difference between those doing 4+ treatments per week, but of those with the lowest BMI, 78.1% did 4+ treatments, while 91.5% of those with the highest BMIs did.
Length of Home HD Sessions

In 2015, fewer than 22% of home HD patients were getting less than 12 hours a week of dialysis. Unfortunately, by 2020, more than 36% were: 44% were prescribed fewer than 3 hours per treatment. The most common home HD session length was 3-3.4 hours (28.3%). A higher percentage of White patients, females, and those with a BMI of below 18.5 were prescribed fewer than 2.5 hours of home HD per session. Patients ages 18-64, males, and those with BMI over 30 were more likely to be doing 6 or more hours of home HD (a total of 4%) than older patients, females and those with lower BMIs.
PD Complications
Good news: peritonitis rates dropped from 13.4% to 5.4% between 2010 and 2020, with lower rates among older patients, males, Asian patients and higher rates in those ages 18-44, females, and Black patients. Bad news: the rate of sepsis nearly doubled, from 6.4% to 12.7%, with higher rates among older patients, female patients, Hispanic and other races, and much higher among people with diabetes (16.7%).
Home HD Complications
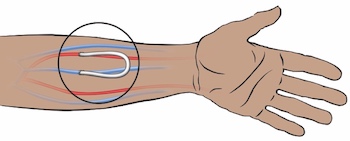
Vascular access* infections declined from 14.4% to 8.6% between 2010 and 2020, with higher rates among younger patients, females, Black patients, and those with other or hypertension as their primary cause of ESRD. Sepsis declined slightly, from 17.3% in 2010 to 16.9% in 2020. Sepsis was higher in patients 75 and older (29.6%) and lowest in those 18-44 (12.3%), similar in females (17.1%) and males (16.8%), highest in White patients (18.9%) and lowest in Black patients (13.3%). Patients with a primary diagnosis of diabetes (19.7%) had the highest sepsis rates.
* Type of vascular access was not specified in this chapter.
Switches from Home to In-center HD
Of PD patients trained in 2018, 23.7% of had switched to in-center HD by 24 months. More of those who switched were younger, male, Black, and with a primary diagnosis of diabetes. Of those starting home HD in 2018, 20.9% had switched to in-center HD by 24 months. Those who switched were more likely to be younger, female, Black or Hispanic.
Transplants Among Home Dialysis Patients
About 12% of those who started PD or home HD in 2018 had a transplant by 2020. Most were younger patients who were White or Asian. More patients on home dialysis got transplants than patients on ICHD.
Questions Unanswered in this Chapter
Are outcomes and patient retention better in clinics with home programs over a certain size, where more experienced staff provide training and support?
Are patients with job-based insurance plans more likely to be using cyclers for PD and to do 4 or more home HD treatments per week?
Is there unconscious bias that prevents older and minority patients from being offered home dialysis?
Why are older PD patients less likely to use cyclers?
Why are some patients getting so little training when fewer training days seems to impact outcomes and reduce home dialysis retention rates?
Are home dialysis patients more likely to get transplants because home dialysis helps patients stay healthier? Or, could bias favoring younger and healthier people to have access to both home dialysis and transplant?
Are there differences in outcomes and type of home dialysis used by those doing PD or home HD in a private residence vs in nursing homes or other institutional settings?
Would providing staff-assisted home dialysis allow more patients to do home dialysis and keep more patients in their private residence rather than living in nursing homes?
Conclusion
Every year I look forward to taking my time and reviewing the chapters and reference tables in the USRDS Annual Data Report. The last two years with reports including a chapter with data specifically on home dialysis has piqued my interest even more. I will be anxious to see what new information is reported in next year’s USRDS ADR.
Reference
United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2022. https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/2-home-dialysis


Comments
Beth Witten
Jul 23, 2025 3:02 PM
https://www.dopps.org/OurStudies/PeritonealDialysisPDOPPS.aspx
I found this study that reports that length of time on PD relates to wait times for transplant. There are a number of other things besides getting a transplant that contribute to how long a patient is able to do PD besides transplant, including infections and declining native kidney function leading to transfer to HD, and death. According to this study, in the U.S. the median time is 2.3 years.
https://journals.lww.com/cjasn/abstract/2022/06000/variation_in_peritoneal_dialysis_time_on_therapy.16.aspx
The United States Renal Data System has data on survival by modality and patient characteristics with adjustment by age, sex, race/ethnicity, and primary cause of ESRD. Tables I.20-I.23 in Reference Table I (survival) showed overall survival, at 1 year was 90.2%, at 2 years 78.0%, at 5 years 67.3%, and 10 years 28.5%. Younger patients had higher survival at each cut point.
https://usrds-adr-api.niddk.nih.gov/api/referenceTables?year=2024&referenceTable=ESRD_Ref_I_Survival_2024
Hope this information is helpful.
Mike Pumo
Jul 22, 2025 3:04 PM