“The Flip”—Helping Patients Switch from PD to HHD

PART ONE: Communication between PD and HHD Needs Continuous Improvement
A Bit of Background…
Last year, I left the bubble of clinical home dialysis “grunt-nursing” and came into the non-profit MEI space where I can focus on writing, education, and advocacy. It’s exactly where I’m supposed to be, I think, because I’ve done the work with my own hands, and naturally look for ways to improve everything I encounter. My perspective lends insight into what needs to be changed in real world practice to make our industry better.
I am actively trying to talk about these things more.
In this post, I have tried to be concise about how we can keep more patients independent, and at home if PD and HHD programs were more closely interconnected. This requires planning and communicating as a stronger team from the way top of clinics all the way down to the staff at the bottom. There’s too much to say to keep this topic short and interesting enough for one post: this is going to have to be a series. So, stay tuned for more…
Eliminating PD and HHD Silos
It seems in our greater community that home dialysis conversations are often split completely in two. There are those firmly Team PD and some very exclusively Team HHD, and that’s that. Who benefits from this mentality? The not-so-hidden rift between PD and HHD is not patient centered at all. These (almost always opinion-based) disagreements on the professional level spill modality biases onto the patients, hindering their ability to make informed decisions. I believe this is wildly unethical. We need to do better than bash any option.
In case anyone reading is wondering, I have “played” for both teams and am proud to be one of the “rare unicorn nurses” to be comfortable and happy to switch between them. There is controversy regarding cross-training of home dialysis nurses, I’m pretty decidedly Team-Knowing-as-Much-as-Possible. I think the flexibility is a huge asset.
I am really lucky to have received 1:1 HHD mentorship for a year with a nurse who had 40 years of experience. I am also really lucky to have been taught PD in the exact same way—from a nurse who remembered when dialysate came in glass bottles and was extremely proud to have never broken one. It was a priceless education to be locked in a small room with those women for 50 hours a week, truly a privilege that I wish more nurses like me had. The deep knowledge of how to actually care for home patients (and keep them home) is slowly being lost, I think. I’ll get to that later, another week.
Plan Ahead for PD Transitions
One thing I find shocking is seeing how often patients return to in-center HD, sicker than ever, feeling wounded, after all PD options have been exhausted. Worse yet, they are fairly often crashing in—as if they weren’t already receiving treatment in the first place. This seems unreasonable. These hospitalizations and their associated traumas can (and really should) be better avoided.
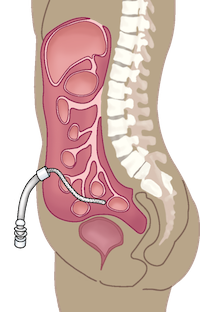
When a membrane is so insulted that no reasonable interventions left will yield adequate dialysis for the patient, it has “failed.” It’s done. It’s exhausted, as are all of the efforts that had been made to keep the patient on the modality. Is it defeating for the entire team, most especially the patient? You bet it is. But, a degraded membrane means the patient is not getting treatment. I hate to state the obvious here, but they still need treatment. A dialysis patient not receiving dialysis due to lack of access is an emergency, not a choice. An inadequate membrane should be taken just as seriously as a poorly functioning fistula. Is it? I’m not so sure.

I would like to see more discussion about transitioning between modalities long before the need actually arises, ideally back when it’s still in the realm of hypothetical complications. I am a huge fan of PD…when it’s working. It really is a bit uncomfortable to emphasize to patients that PD is a temporary modality when they’re finally feeling like life is getting back to something resembling normal, but pretending that the elephant doesn’t always have the chance to walk into the room is a missed opportunity.

We can give better service when we plant the seeds for modality conversion early, with the objective of keeping each patient independent and at home, for as long as possible, whenever possible. If we’re looking at total home patient census, especially on the “long-haul” patients, identifying who would be a candidate to “flip” to HHD in the hypothetical future isn’t unreasonable or even very difficult.
For those of you who are reading this and are training and following home patients:
Are you discussing potentially declining membrane plans at your IDT and QAPI meetings?
Are your nurses cross-trained and wildly competent?
Are your PD nurses friendly with your HHD nurses and working together to hold the census? They really ought to be, it’s good for patients to have them (at the very least) functioning as a team.
Ban Cross-modality Bashing

Cross-modality bashing needs to become taboo within home departments. Scaring patients isn’t helping. PD nurses have a responsibility to demystify HHD while they have the opportunity. Yes, the needles are quite large. Don’t impart pre-emptive trauma on people who will likely have to face that as a reality someday.
The home staff, both on the PD and HHD side, need to know who is in the pipeline for possible modality shift and need to plan for where these re-trainings can be scheduled in. HHD programs should be aware of which PD patients are struggling and facing a functional end of modality. They should be mutually followed. You can teach slowly and build knowledge when you know you have some time before you need to make a “flip.” This is much easier to schedule.
Anticipate and Communicate

Care teams can be—and need to be—better at anticipating the need to re-evaluate modality choice prior to “membrane failure.” It is okay to recognize and articulate the earliest signs that PD is no longer working optimally. The patient needs to be aware of why this happens, how this process works, and a discussion needs to take place where it is made perfectly clear when decisions will have to be made.
These conversations can be really hard. But people need informative support, so there can be a plan in place before there is a crisis. There is no reason to let crises happen.
Normalize the anxious feelings associated with change, and promote resilience and hope. This dialogue needs to be continued if we want to improve utilization of home therapies. When the goal of care is an independent, functional, and self-sufficient home patient, there is no disconnect between PD and HHD. We have the same priorities and need to be much more closely connected.
Next time, I’ll talk about how to trouble-shoot PD complications while laying down the foundations for HHD at the same time. Stay tuned for that if you’re interested in hearing more about how we can better accomplish “the flip” from PD to HD seamlessly!


Comments
Susanne Noble
Aug 26, 2024 5:58 PM
Kat
Jul 29, 2023 9:23 PM
So I'm trying to plan ahead for myself..looking into all my choices if I ever need to be faced with making a decision.
Thank you for this article
Tina M Renfroe
Jul 18, 2023 3:02 PM
Nancy Verdin
Jul 13, 2023 5:04 PM
Steve
Jul 13, 2023 4:39 PM