The Rainbow of Peritoneal Dialysis Effluent Possibilities

Originally published on January 04, 2024.
When discussing complications of PD, there is no shortage of information about infection-related issues such as exit-site-infections and peritonitis. These are relatively common occurrences and require immediate medical management. There is also no lack of advice regarding managing mechanical dysfunction in PD—like how simple constipation can stop-up the entire show, how much heparin to use, or the many ways to manage pesky drain pains.
Those who are just starting off learning PD are bound to come across some interesting things as they go, but the nuances of discolored PD effluent are a concern many newer nurses have not seen before, or even heard of yet.
Since this is a conversation we have been having recently with patients on our Home Dialysis Central Facebook group, I thought it might be a good idea to talk about what PD effluent should and shouldn’t look like and hopefully explain some of the oddities possible.
Clarity Matters
Let’s start with the most basic rule: all peritoneal effluent should be clear. Effluent that is not crystal clear (see-through) and a normal yellow color needs to be reported immediately and the cause identified.

What is CLEAR? When we say that the fluid should be clear, we are referring to the clarity of the fluid, not the color. I always feel like I’m explaining how diamonds are graded when I teach this difference, but once you think of it in that context, it’s much easier to visualize.
Crystal clear fluid means you can read printed text through it. If the fluid is hazy and you are unable to see letters through the bag, the fluid is not clear.
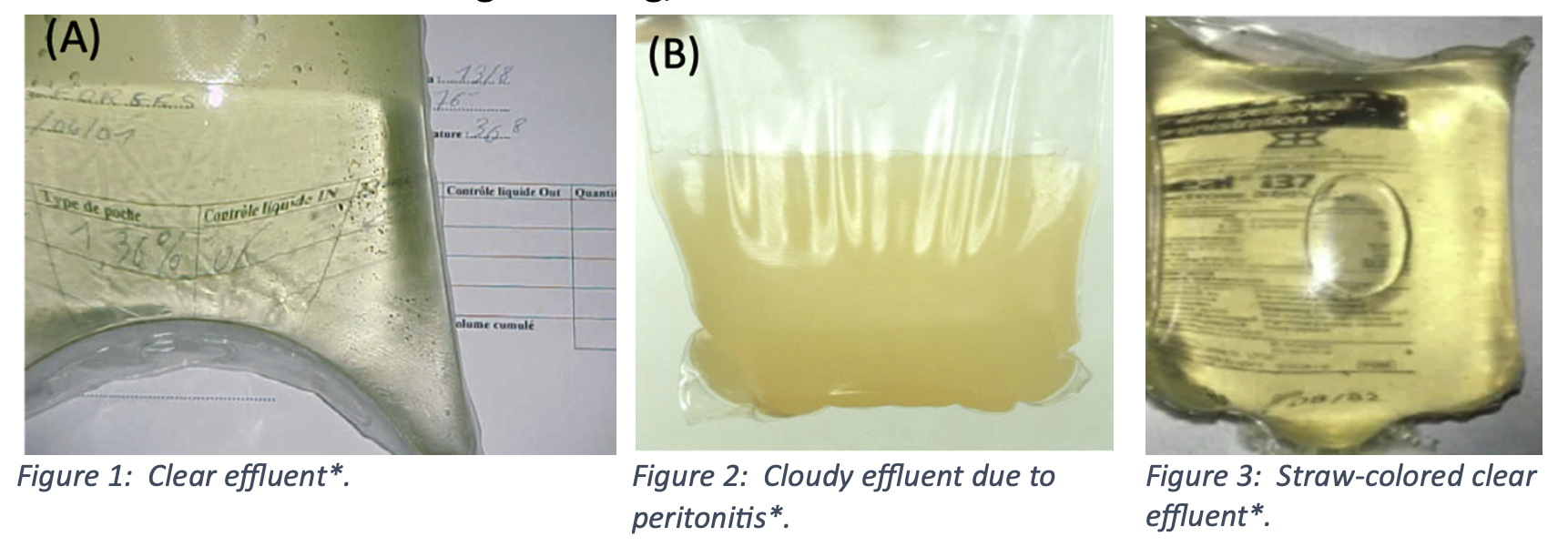
What is CLOUDY? Again, we’re talking about clarity here, not color. If drained fluid is too turbid to read through, it is cloudy, and that warrants an immediate work-up for peritonitis. Every patient, care partner, and staff member managing PD should immediately say “PERITONITIS!” when presented with cloudy fluid.
There can be noninfectious causes of cloudy fluid, but until infection is ruled out, the assumption of peritonitis must be made to preserve the membrane. The cloudy appearance is caused by infection-fighting white blood cells.
PD Effluent Color
Peritoneal effluent contains electrolytes and uremic toxins. If it has been dwelling for a while, the drained fluid should be a straw-yellow—like urine. Effluent that has been dwelling for a long time may be darker than fluid that was recently instilled. Hydration status plays a role in how dark or lightly colored effluent is, too. When effluent does not look as expected, there is a reason:
RED PD Effluent: This is hemoperitoneum. If you are a PD nurse, before you send any younger female patients home on PD, ask yourself if they might ovulate or menstruate at some point. This doesn’t even have to be a regular occurrence, just a general possibility. If the answer is in any way affirmative, the patient needs to be told that releasing an egg, or shedding some endometrial lining can (and really does) cause bleeding into the peritoneum. The dwelling fluid then turns bright red. This sight can be completely shocking and horrifying if the patient has not been warned. It really looks like a lot of blood.
You can suggest irrigating the peritoneum with cool dialysate or filling with cool fluid to discourage further bleeding. If clots are present, your patient may need to add heparin to keep catheter flows smooth.

There are other reasons for effluent to be bloody that aren’t as normal and need to be evaluated. If the cause of the bleeding is not routine and gynecological, the reason needs to be found. A ruptured cyst (ovarian, renal, pancreatic, hepatic, etc) can bleed into the peritoneum and cause pain and/or profound bleeding. In addition to cysts, some types of cancers and tumors can bleed internally in the same way and show up unexpectedly in a drain.
Ruptured vessels can present this way too. Typically this happens from a minor irritation (exercise or heavy lifting) and the internal catheter rubbing on structures causing microtrauma and capillary bleeding. Major vessel bleeds, like ruptured abdominal aortic aneurysms can cause major life threatening hemorrhage and bleeding into the peritoneum. This type of medical emergency is not caused by dialysis, but the symptoms can be seen because of it.
ORANGE PD Effluent: The antibiotic Rifampicin is used to treat mycobacterial infections and tuberculosis. It has a side effect of turning bodily fluids (tears, sweat, urine) orange. PD effluent is affected by this too, and this might happen with other medications that change body fluid colors. If a patient is prescribed a medication that has the potential to change the color of their urine, it may also change the color of their effluent even if this is not a known or stated side effect. They should be made aware of the possibility before it causes unnecessary panic.

RUST PD Effluent: If a patient on PD receives rifampicin and IV iron together, the effluent from the antibiotic-iron combination turns a rusty shade of orange-red. This is a harmless side effect.
BRIGHT YELLOW PD Effluent: Liver failure, some cancers, or heart failure can cause extra free fluid to build up in the abdomen. This can be very uncomfortable, depending on how much fluid is produced. In the non-dialysis population, a full abdomen can be drained with paracentesis—a tube is placed into the peritoneum temporarily to relieve pressure. For those on PD who also have ascites from liver failure, the peritoneal catheter offers a sterile and regular manner to drain the fluid. This may not look very different from regular effluent, but may be brighter yellow in color, with more volume present than expected.
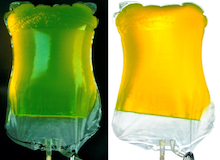
FLOURESCENT YELLOW-GREEN PD Effluent: The first time I saw glow-in-the-dark effluent, I thought my patient was playing a trick on me! I was in my office, and suddenly there was a very alarmed man standing in my office holding a 3000 mL bag of effluent that was so fluorescent, it looked radioactive. He had just finished draining at home and ran right in so fast that the fluid was still warm.
I had read about this before, and instantly knew what I was looking at, but was really surprised that it was as…bright and vibrant as it was. It’s remarkable: like the liquid inside of a glow-stick. Anyway, even though it is a very cool thing to get to educate about after it has happened and you have a giant bag full of proof that diffusion really happens, it’s something everyone should be aware of, lest you wonder if your patient is turning into Spiderman. It actually does glow in the dark—I checked! I had read that “some contrast dyes” can make it into the peritoneal space, but since I had never seen it happen before, was completely stunned. My patient had had an eye exam for glaucoma, received IV fluorescein contrast, and dialyzed it out through his peritoneum. Pretty neat, really, especially since it does not cause harm.

GREEN PD Effluent: Effluent that is yellow-green-brown points to a leak of bile into the peritoneal cavity. Any leak in the GI system is a risk for infection and may indicate that the patient has cholecystitis that has perforated. Bile is green, and if there is any leak in the biliary tree system, the effluent can turn green. The hue can be dark and muddy. It doesn’t look healthy, which is a really good tell that it needs further evaluation right away.
GREEN PD Effluent with PARTICLES: can indicate a perforated ulcer that is leaking food and gastric juices into the abdomen.
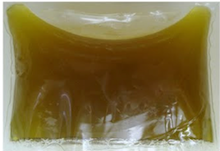
BROWN-GREEN PD Effluent with PARTICLES: If effluent is brown or green with particles mixed in, it is possible the patient has a perforated bowel and feces are leaking from the gut and mixing with the dwelling fluid. Any leaking from the GI system into the peritoneum is going to cause an infection if it hasn’t already—so there are multiple things going on when this is seen.

BLUE/PURPLE PD Effluent: A few years ago, PD patients in Europe were stunned when they began to drain and saw that their effluent was a strange shade of purple or blue. An investigation discovered that iodine in the PD catheter caps was reacting to Extraneal PD fluid manufactured in Turkey. No harm came from this, and it has not occurred since 2011.
CLEAR BROWN PD Effluent: “Coca-Cola” colored effluent is a sign of hemolysis. This can happen with pancreatitis, when enzymes mixed with blood break down the cells, or with rhabdomyolysis. Both are different from hemoperitoneum, as the red blood cells have been destroyed.

BROWN-BLACK PD Effluent: Similar to the green effluent, dark brown to black fluid indicates that bile is leaking. There may also be bilirubin present, which can be tested for. The green color from bile and the red-orange-yellow pigment from the bilirubin combines to create very dark fluid. If the effluent has more bilirubin than the blood does, the patient will most likely need an emergency exploratory surgery to find the source of the leak. A gangrenous gallbladder or pancreatic complications are possible.

MILK WHITE PD Effluent: We are programmed to think of any opacity in PD fluid to be “cloudy” and thus indicating an infection. This isn’t always the case. Some effluent can be MILK WHITE and completely opaque. This looks just like lipids—because that’s what it is. High levels of triglycerides and a blockage of lymphatic chyle drainage from the intestines causes fluid build-up into the peritoneum. This can happen as the result of a high fat meal, trauma, or severe diseases like lymphoma and congestive heart failure.

PEACH/PINK PD Effluent: What do you get when you mix hemoperitoneum and a chyle build-up? I’m not sure if there’s a word for this specifically, but the effluent can look peach or pinkish in color when they mix. The cause of the bleeding and lymphatic back-up need to be identified.
BLACK PD Effluent: As a heavily tattooed nurse, one of my favorite ice-breaking conversations with new PD patients is one I was told about many times by older-generation PD nurses. Apparently, during colonoscopies, medical tattoo with India ink is sometimes used to mark an area for future surveillance. Ink transfer through the peritoneum is rare, but is something PD patients and staff should be aware of.
I hope this post makes it a little bit easier for those involved with PD to know what they’re looking at when presented with an inevitable oddly-colored drain bag. In writing this, I noticed there was very little quick and easy information out there about effluent anomalies with photographic examples. The links to the articles containing the photos used are listed below for reference.
Image sources are as follows:
Figures 1, 2, 4, 5, 6, and 10: https://onlinelibrary.wiley.com/doi/10.1111/sdi.12740
Figures 3 and 12: https://nephsim.com/case-10-diagnosis-conclusions/#CaseIndex
Figure 7: https://www.renalfellow.org/2010/02/01/green-peritoneal-dialysis-fluid/
Figure 8: https://doi.org/10.1186/s12882-018-0974-6
Figure 9: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3707724/
Figure 11: https://www.kidney-international.org/article/S0085-2538(20)31543-X/fulltext


Comments
Pamela Robinbson
Oct 24, 2025 7:24 PM
Donita Rostock
Nov 29, 2024 5:37 PM
Maria Melling
Jan 17, 2024 5:41 PM