View from the Chair: Why Did You Choose Your Dialysis Option?

As you can imagine, at MEI, we spend a lot of time observing and thinking about the decision-making processes used by people who face the need to choose a type of dialysis, either while waiting for a transplant or if they don’t qualify for or want one. Keep in mind that no one wants to need dialysis, any more than anyone wants to need chemotherapy or radiation. NONE of the modalities tend to look good to those who need them! So—as with many elections—the choice may be a matter of the least-bad option. A recent social media thread illustrates that we still have quite a way to go before modality choices are made in a way I would consider ideal: by considering what matters most and choosing an option that will give people the lives they want.
Why Not Home?

Let’s start with reasons some people gave for “choosing” standard in-center HD. I use the quotation marks because a lack of real choice was a theme, despite a Medicare rule since 2008 (16 years now!) requiring clinics to inform patients about ALL of their options and where to get them, including options a clinic does not offer. This is still not happening—in particular, it’s quite clear that home HD is an option some remain unaware of:
“No choice in hemo no kidneys.”
“Only way for me to go.”
“I had no choice but hemo, because my peritoneum doesn't absorb properly.”
“No choice after pd failed.”
“I didn’t have a choice, I was on PD but had to have my catheter removed, so now I’m on hemo.”

In some cases, a forced HD choice occurred due to PD issues—catheters, failure to meet adequacy standards, etc. Even so, transfers to home HD were seldom mentioned:
“Pd did not work it was a disaster.”
“How well I was hitting my clearances. I was on PD for a year but it didn’t work so I’m on in center hemo now.”
“Had done the tube stuff before my first transplant. Dr in the hospital recommended I use hemo now.”
“I am currently sticking with in center hemo because I did PD years ago and kept getting peritonitis. Then it became a fungal peritonitis and they said I couldn’t do PD any more. Home hemo sounds attractive in terms of feeling better, but it sounds very time consuming, and I don’t want to put my old fistula through the wear and tear of venipuncture more than 3 times a week. I would love in center nocturnal hemo 3x/week, but the closest place is an hour away.”
In other cases, fear—of supplies in the home, self-cannulation, or “something going wrong”—led people to make the seemingly “safe” choice of standard in-center HD—likely without knowing that the outcomes for this option are objectively poorer than for home HD and, in the U.S., are far worse than in Canada, Europe, Australia, New Zealand, and, especially, Japan:
“Do the wacky stuff at center. so that at home, out of site out of mind. I could not see that in my house with 4 Grandkids. very Mental.”
“I can't self stick and pd was not a option and gets me out of the house.”
“i like being there in case something goes wrong. and the fact that the clinic is only a five-minute drive.”
Finally, instrumental concerns largely about supply storage in the home scared some people away from PD:
“I'm paying the big bucks for my insurance I'm going to have someone do it for me. And dint want my room to look like a supply house.”
“I don't have space in my house
 .”
.”“I no longer had a lifestyle or living space that would support peritoneal dialysis.”
“It worked best for my life. My house is my sanctuary and I don't want a lot of medical stuff in My Sanctuary. So I now go two days a week in clinic.”
Reasons for Choosing PD or Home HD
FREEDOM & CONTROL
A theme that came through loud and clear was wanting to regain control over a life that may have been derailed by a chronic illness where all of the treatments are time-intensive and some have other restrictions as well.
-
“I chose home hemodialysis because of the freedom.”
-
“Work. I can’t be missing work to come do dialysis. At least with PD, I have the freedom of doing it whenever I can.”
-
“Initially I wanted to do PD but a couple major abdominal surgeries put the kibosh on that. I had heard about nocturnal hemodialysis years before starting dialysis and talked with my nephrologist about it, but she told me it wasn't safe to do alone. When it came time I started in center because everyone told me solo home hemo wasn’t safe. About 1.5 years in I asked the FA about doing self-care in center and when she expressed excitement about that I told her I really wanted to do home hemo, but lived alone. She thought I'd be the ideal candidate for solo HHD and she talked the training nurse in to training me. It's been almost 8 years now.”and I have no desire to go back in center. It's a lot of work and there have definitely been some challenges but I like making my own schedule and changing it on the fly. I like being in charge of my treatment.”
“Chose pd because I like to pack up and travel whenever I wanted. I didn't wanna mess with blood & needles and I like the fact I can sleep through it and be done in the morning.”
“I chose to do PD after I was on hemo for 9 years. I definitely prefer PD. No blood, no needles, I do it at home, no fluid restriction, I can eat as many potatoes, tomatoes, and avocados as I want, no nurses or techs trying to rule my treatments.”
“Home Hemo because PD freaked me out. Doing it at home because of awful experience with in-center treatments.”
“Did hemo for 5yrs (before getting a transplant) (after transplanted kidney failed) i did hemo again for about a year but it wasn't the same because ZERO output so i tested pd and after about 2 to 3 months of bumps it's been great. Numbers are great and I can do it at home. don't have to notify the center 30 days prior to vacation.”
“Home hemo, my clinic is not close and I like being on my own schedule.”
Better Treatment/Outcomes
Not everyone was unaware of the benefits of home therapies for wellness and lifestyle. Some chose PD or home HD deliberately to have the best chance of living well and fully.
(Home HD). “Reading, learning and implemented all new and the best. Thanks to that I am 43 years on dialysis in very good condition.”
“Pd, I took for the freedom to work, hated it. In center, to remove more toxins and feel better. Home hemo, more freedom, can work with all the benefits of in center, but no travel, less hours on the machine, less pull.”
“I wanted the best treatment there is, and the benefits I receive. And my family is involved and don’t have to be afraid of what’s happening. Nxstage Nocturnal Home Hemo for me is the best out of them all.”
“Nocturnal is best and easiest on body.”
“Nocturnal HHD because it gives us better lab work and gives us no recovery time and our days and evenings back.”

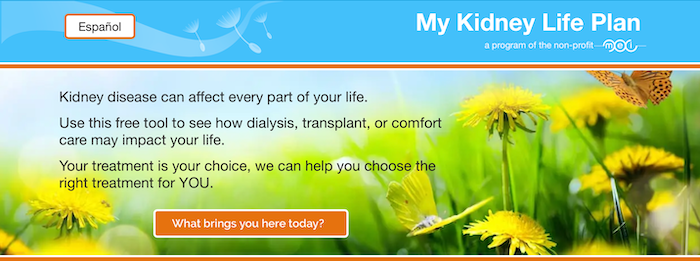
A Free Tool to Match Options to Patient Values
If YOU had to choose a treatment for kidney failure, wouldn’t you want a way to sort out what is most important to you—and then help to match a treatment to what really matters? My Kidney Life Plan is a decision aid—or treatment matcher—to do just that. Developed to meet all of the International Patient Decision Aid Standards (IPDAS) criteria, this tool is written at a 5th grade reading level and includes evidence-based information about transplant, seven types of dialysis, and conservative management.
We recommend that My Kidney Life Plan be used FIRST, to instill critical HOPE—BEFORE potentially scary detailed information about modalities. The summary page can be added as an Advance Directive to patient medical records, and helps guide more productive conversations with clinicians. Using the tool may increase patient willingness to attend CKD education classes and make an active, informed choice that lets them live their best lives.


Comments