March Is Kidney Month and Social Work Month

Did you know that March is not only National Kidney Month, but Social Work Month as well? The 120,000 member National Association of Social Workers (NASW) collaborated with Rob Lowe on a mini-documentary to promote mental wellness and encourage greater access to behavioral health services in healthcare settings.
Kidney disease is unique in that the federal government recognized the importance of addressing mental wellness in dialysis. The ESRD Conditions for Coverage (CfC) REQUIRE every dialysis clinic and every transplant program to provide patients access to a social worker with a master’s degree in social work who is licensed, if required, in the state where they practice. Dialysis social workers participate on an interdisciplinary team (IDT) that also includes the patient, physician, nurse, and dietitian. Under the ESRD CfC at 42 CFR 494.80(a)(7), social workers are explicitly charged with assessing the “psychosocial needs” of all the dialysis clinic’s patients. According to the World Health Organization 30-55% of health outcomes are related to SDH. On its website, it defines SDH this way:
“The social determinants of health (SDH) are the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life…“The following list provides examples of the social determinants of health, which can influence health equity in positive and negative ways:

-
Income and social protection
-
Education
-
Unemployment and job insecurity
-
Working life conditions
-
Food insecurity
-
Housing, basic amenities and the environment
-
Early childhood development
-
Social inclusion and non-discrimination
-
Structural conflict
-
Access to affordable health services of decent quality.”
Nephrology social workers have known this for decades. The Interpretive Guidance (IG) to the ESRD CfC lists some but not all of the areas that social workers assess:
- Cognitive status and capacity to understand
- Ability to meet basic needs
- Ability to follow the treatment prescription
- Mental health history, capacities, and needs for counseling
- Substance abuse history, if any
- Current ability to cope with and adjust to dialysis
- Expectations for the future and living with kidney failure and treatment
- Educational and employment status, concerns, and goals
- Home environment including current living situation
- Legal issues (e.g., court appointed guardian, advance directive status, and health care proxy)
- Need for advocacy with traditional (nursing home) and non-traditional housing (e.g., homeless shelters, group homes)
- Financial capabilities and resources
- Access to available community resources
- Eligibility for Federal, State, or local resources
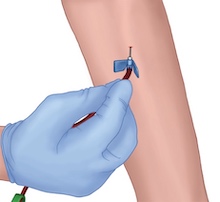
Besides clinical areas, the IDT is to assess “the patient’s abilities, interests, preferences, and goals, including the desired level of participation in the dialysis care process; the preferred modality (hemodialysis or peritoneal dialysis), and setting, (for example, home dialysis), and the patient’s expectations for care outcomes.” The IG requires the staff to evaluate and consider self-care training for patients who want to monitor their weight, BP, hold their needle sites or self-cannulate. Self-cannulation can be a steppingstone to in-center self-care or home HD. The social worker can also assist the IDT assessment by evaluating the patient’s support system and need for vocational and/or physical rehabilitation.
Once the IDT has completed its assessment, the next step is for the professional members of the IDT to collaborate closely with the patient on a plan of care that addresses his or her individual needs. Social workers take the lead on the plan for “psychosocial needs” [42 CFR 494.90(a)(6)]. They can provide counseling to help patients (home and in-center) “achieve and sustain an appropriate psychosocial status” and to identify problems related to patients’ health-related quality of life (HRQOL). Social workers ask patients to complete (with or without help) a validated survey such as the PedsQL for those under age 18 or the KDQOL-36 for those 18 and older. The KDQOL-36’s five domains include physical functioning, mental functioning, symptoms/problems, burden of kidney disease, and effects of kidney disease on daily life.
Medical Education Institute (MEI) developed KDQOL Complete (KC) to help clinics score and analyze survey results, generate a report to inform the patient’s Plan of Care, and provide patients with suggested ways to improve their scores. KC also provides multiple clinic reports the IDT can use for quality assessment and performance improvement (QAPI) meetings. It monitors how many patients completed surveys for the month and year vs. the prior year, survey refusals and exclusions, demographic and treatment data, plus the HRQOL status by domain of all of the clinic’s patients surveyed.
Discussing scores and goals with patients and reviewing their answers to individual questions within each domain can help the IDT plan how to maintain scores that are average or above while addressing below average scores. This is important because more than two decades ago, research found that dialysis patients are at greater risk for hospitalization and death if they have low HRQOL scores.1 Social workers who used Symptom Targeted Intervention (STI) techniques and tools reduced depression and improved HRQOL.2
Patients who do in-center dialysis may see their social worker regularly. But those who dialyze at home may not be aware of all the ways their social worker can help them. The National Kidney Foundation (NKF) published a fact sheet that social workers can share with those on in-center and home dialysis to make sure they know the social worker’s role. Although social workers do help those who do dialysis to understand options to pay for dialysis-related expenses and how to access financial resources, they do much more, such as:
- Counseling to help patients and families—including care partners—to cope with kidney disease and dialysis
- Patient referrals (with MD orders) for home health and physical rehabilitation
- Encouraging patients to stay engaged with their friends, families, and communities
- Helping patients identify and work toward vocational goals, with referrals as needed
- Helping to address conflicts, complaints, and grievances
- Serving as the patient’s advocate with the IDT; and much more
Social workers are invaluable members of the IDT. They help the rest of the IDT to educate and support all patients, including those on home dialysis. Social work interventions empower patients to work toward achieving their goals. Dialysis social work is not an easy job, with large numbers of patients and limited time to meet their needs, however for many long-term dialysis social workers, it is a calling. This March during Social Work Month, I call upon all dialysis patients and staff to make a special effort to thank your social worker for all s/he does.
Mapes, D. L., Lopes, A. A., Satayathum, S., McCullough, K. P., Goodkin, D. A., Locatelli, F., Fukuhara, S., Young, E. W., Kurokawa, K., Saito, A., Bommer, J., Wolfe, R. A., Held, P. J., & Port, F. K. (2003). Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney international, 64(1), 339–349. https://doi.org/10.1046/j.1523-1755.2003.00072.x↩︎
Sledge, R., Aebel-Groesch, K., McCool, M., Johnstone, S., Witten, B., Contillo, M., & Hafner, J. (2011). Part 2. The promise of symptom-targeted intervention to manage depression in dialysis patients: improving mood and quality of life outcomes. Nephrology news & issues, 25(7), 24–31.↩︎


Comments