Improving Access to Home Dialysis: My Testimony

There are still many barriers to providing access to home dialysis for the nearly 540,000 patients on dialysis. All patients deserve to know all options for dialysis and that some may offer better opportunities for improved quality of life and lower mortally risk. The National Kidney Foundation estimates that only 14% of patients on dialysis in the US are using at-home options.
The Improving Access to Home Dialysis Act (HR-8075) was recently introduced in the U.S. House of Representatives by Reps. Carol Miller (R-WV), Marilyn Strickland (D-WA), Earl Blumenauer (D-OR), and Mariannette Miller-Meeks (R-IA). Before its introduction, the House Ways and Means Committee chaired by Rep. Jason T. Smith, Missouri, held a hearing in March entitled: Hearing on Enhancing Access to Care at Home in Rural and Underserved Communities. This was my written testimony.

Thank you Chair Jason T. Smith for the opportunity to provide written testimony in support of enhancing access to care at home in rural and underserved communities. I have been on home dialysis since 2001 and I am passionate about the benefits of home dialysis and its positive impact on lifestyle and decreased mortality risk. Because of the energy that I have with doing home dialysis versus three times a week in-center dialysis, I’ve been able to be a long time advocate for other patients looking to find their best life with End Stage Kidney Disease (EDSK) while on dialysis.
I’d like to share some of my personal journey while listing some observations that I have made over my nearly quarter of a century of dialyzing at home. While there have been significant struggles for me, my wife, and our children along the way, including for my personal ones of depression, early on suicidal thoughts, difficulties with anemia, a couple issues with infections, and problems surrounding the burden of home dialysis, I wouldn’t have it any other way. I’m able to write this letter and share my thoughts with you and the Committee, because home dialysis has been my “Gift of Life”. The positives of home dialysis have far exceeded any negatives that we have had to endure. While the details are compelling, I will save them for another time and keep my observations short and to the point.
1. New dialysis systems have made home hemodialysis easier
I first started home hemodialysis in 2001 thanks to the foresight of my
University of Michigan (UofM) dialysis clinic nephrologist. To have it
in my house I had to add a pressure regulator and pump to my plumbing to
ensure the appropriate pressure from the street to the newly installed
reverse osmosis system. This system supplied clean water to my full size
dialysis system which used it to make dialysate which the machine used
to clean my blood and remove excess fluids. At this time, this was the
only way to do home hemodialysis. Now we have two different FDA
approved home hemodialysis systems, each with their own much smaller
water purification systems that don’t require extensive plumbing
additions.
Now we have two different FDA
approved home hemodialysis systems, each with their own much smaller
water purification systems that don’t require extensive plumbing
additions. This allows for smaller footprints and easy and lest
costly setup. Also, the supplies one would have to store in our house,
from one manufacturer which received federal approval for their machine
in the early 2000’s were greatly reduced because of its 2008 water
purification/dialysate production system. Innovation is needed to
make dialysis machines that are easier to transport, simpler to operate,
and that will allow for more flexible prescriptions.
This allows for smaller footprints and easy and lest
costly setup. Also, the supplies one would have to store in our house,
from one manufacturer which received federal approval for their machine
in the early 2000’s were greatly reduced because of its 2008 water
purification/dialysate production system. Innovation is needed to
make dialysis machines that are easier to transport, simpler to operate,
and that will allow for more flexible prescriptions.
2. There is a burden on the user and the care partner
Using that full sized machine put a particular burden on my wife, Andria, who trained to operate the machine and was now my care partner in a way that we had never imagined when we fell in love at the age of sixteen years old. After ten years of enduring miscarriages and infertility, we were fortunate to have adopted our son, Jacob, when he was born. We had recently moved to East Lansing, Michigan for my new job, and Andria had planned to stay home to care for Jacob. When I switched from in-center three times a week dialysis to our new home system provided by U of M in-center dialysis clinic, I went back to work. My dialysis prescription called for me to do dialysis five days a week which made me feel much better. But at that time Andria took care of most of my dialysis needs. She would set up the machine, cannulate me, hook me up to the machine, respond to any alarms while tending Jacob and making dinner. The she would take me off the machine, disinfect the machine, and finally break it down. This was a lot of work, but it allowed me to continue to make a living for are our family. When we travelled, I would go into a dialysis center nearby to where we were staying. This gave Andria a well needed break from keeping me alive, but it kept me away from them for at least five hours on the three days I dialyzed. Care partners need support in their duties and the opportunity for respite.
3. It is important for the person dialyzing to participate in their treatment to the best of their ability
After a while dialyzing more frequently with the full size machine, with Andria doing nearly all the work, I felt stronger, more independent, and I had more energy. I came to realize for me to feel this way that I was placing a huge burden on Andria. While she said I do to our vow of in sickness and in health, I knew she hadn’t signed up for this.
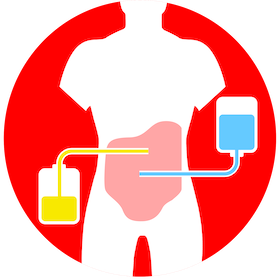
I talked with my nephrologist who then prescribed peritoneal dialysis (PD) for me. This time I said yes. When I first crashed into dialysis at the end of 2000, this same nephrologist had suggested that I consider starting with peritoneal dialysis (PD). Now this was rare in the early 2000s to be provided to start on PD so early in the need for dialysis. At the time and even now, many patients are simply sent to in-center dialysis without being made aware of home modalities.
After they explained the first time that they would place a catheter in my belly and that I would have to do PD every night with a bedside machine while I slept I felt it was too daunting. I also was uremic at the time, feeling the symptoms of too many toxins in my blood–one of which is a brain fog. Also, knowing then that I would have a transplanted kidney in five months, it seemed like too much work compared to three-times-a-week. I didn’t realize at the time that I would feel much better with daily dialysis. That the toxins and fluid would be taken out much more frequently and not be allowed to build up as with traditional in-center dialysis. But, once I was cleaner and stronger due to more frequent home hemodialysis, and the transplant that I received from Andria immediately shut down due to the disease primary focal segmental glomerulosclerosis (FSGS), I realized the PD would greatly help our family and still allow me to work. Even though it was a huge storage of supplies burden, I felt great and the ability to travel with it allowed me to stay with my family on vacations. Heck I even did manual exchanges of dialysate inside the Magic Kingdom’s first aid room while on a family trip. With PD as my system, Andria and I adopted our daughter, Antonia, from birth in another open adoption. This was during my fourth year of home dialysis. Dialysis patients need to be given the opportunity to take control of their dialysis options in order to improve their quality of life.
4. We must remove racial disparities in dialysis

When I crashed into dialysis, I was a thirty-six year old man living in East Lansing near the capital city of Michigan. Because our son and our daughter are both Black, I was learning about my white privilege. I will soon be fifty-nine. When I first found myself on emergency dialysis, I also found out at the time that the average life-span on in-center dialysis was seven years. With home hemodialysis, my wife and I were fortunate to expand our family and be there every step of the way through their high school graduation and into them becoming the incredible young man and young woman they are today. Through this journey I am now completely aware that my white privilege has made my opportunity for transplant and for my longevity on various means of home dialysis possible. Whether this played a role with my own personal providers I cannot tell, though I am doubtful based on the individuals that I came know, but rather it may have played a role in systems in which they were working within the dialysis community as a whole. My family is now made up of two white adults and two black adults. I want to ensure that my children, who because of their ethnicity are at a higher rate of acquiring kidney disease, will not suffer through racial disparities to get the same treatment if needed that I received.
5. Lower mortality risk matters
I used PD up until I received a deceased donor kidney in 2005. Because of the lack of donated kidneys, I was fortunate to join the waiting list in two different states for a kidney transplant. This isn’t the case for everyone in need of a transplant. The barrier of distance often can’t be overcome due to access to and means for transportation. I received my new kidney transplant at the University of Wisconsin Hospital in Madison, where unfortunately the primary FSGS began to shut it down immediately. After six-weeks undergoing plasmapharesis, it later was infected, and like the kidney donated by Andria, was surgically removed. For many of the over 500,000 people on dialysis in the US, transplants may not be an option. And for us, dialysis is our gift of life.
I came back to East Lansing and began in-center dialysis with a large dialysis provider organization. Soon after starting, I learned about a rather new transportable hemodialysis machine which used sacks of dialysate, similar to the PD machines. This allowed for travel without having to go in-center. I spoke with my new nephrologist about it and she agreed that I would make a good candidate. My current dialysis center didn’t offer it and I had to got to a center operated by a different large dialysis provider organization in Flint. This center is nearly an hour away by car. Again, fortunately I had the means to make the daily commute for the next three to four weeks for training. Since I was no longer working due to disability based on ESKD, I also had the time to do the training. If I had still been working, their daytime schedule would have been difficult for me to attend. With this training, my wife had to take time of work for a week to be trained on this system. It was my plan to do this type of home hemodialysis independently with Andria being there as back up if needed. And that is how it has been.

After three days of training I felt significantly more energy. I did dialysis six days a week at a time of my choosing that worked for our family for about two and a half hours each treatment. I was even more active with our children than on PD. Two years after starting with this new machine, I learned from other users that nocturnal use would be even better by being gentler on my heart, cleaning toxins that were hard to remove at higher speed more frequent dialysis, and would free up my days. Again with my nephrologist’s backing and support, I switched to a small dialysis provider organization in downtown Detroit. After just a week of training for some additional safety procedures, I started doing home hemodialysis for eight hours five nights a week while I slept next to my wife, with the kids asleep down the hall in their rooms. Research has shown that nocturnal home hemodialysis provides the same mortality risks as does a deceased donor transplanted kidney. My goals from day one of dialysis back in 2001 were to live an incredibly good quality of life for a long time. And that is what I am doing with nocturnal home hemodialysis.
In closing, despite the lofty goals for having ESKD patients to adopt home dialysis as spelled out in the 2019 Kidney Health Initiative, there are still many barriers to home dialysis uptake including the following:
Inadequate level of training and exposure among nephrology professionals.
Care partner burnout.
Inadequate information and training of patients.
In adequate number of home dialysis centers.
In adequate number of staff to train those wishing to switch to home dialysis.
Access to transportation to training at home dialysis centers.
Lack of available assistance to those wishing to dialyze at home but may not be able to physically preform it on their own.
Rules requiring only nurses to provide the training.
These must be tackled to ensure that all ESKD patients can have the goals of living a good quality of life for a long time. I look forward to working with you and your fellow Committee members and others to address these barriers to improve home dialysis access care to rural and underserved communities.
Thank you for your time.
According to the National Kidney Foundation, the Improving Access to Home Dialysis Act will:
Mandate that patients get proper education on all of their dialysis options, including making sure that even patients who crash onto dialysis with no preparation can get education on other options once they have stabilized and can make informed decisions about their future.
Expand the universe of healthcare providers who can provide home dialysis training to remove the burden from the nursing staff and cut down on wait times to get trained. It would also allow for the use of group training, telehealth, and off-site training when appropriate.
Cover the costs of in-home healthcare support staff for patients when they are beginning their home dialysis journey. This in-home assistance would help patients transition from the facility and support the patient and if available, their care partner, with the goal that they become fully independent over time. Some patients with certain disabilities or other concerns could be eligible for continuing in-home assistance.


Comments