Less Hemodialysis is NOT More

In the past couple of weeks, two similar questions popped up in different Facebook groups:
“I have a question. Have any of you that do 3 days a week decided to just do 2 days? Do you feel better or worse? I’m think of just going Monday and Friday.”
“Anyone here do HHD 3 days a week?”

Re: two days a week, other dialyzors noted that:
Missing treatments can reduce the chance for a transplant.
Nephrologists prescribe dialysis and patients can’t just decide to do fewer treatments.
“U miss u shorten ur life.”
“If you start doing 2 days instead of 3 after awhile fluid will start to accumulate in the lungs and you will have shortness of breath.”
Re: three days of home HD per week, other dialyzors noted:
“I did every other night so some weeks I had three some weeks I had four. That being said I did nocturnal so I was getting 8 hours when I did it.”
“5 days hhd so much happier.”
“Our nephro said that defeats the purpose of doing HHD. He says home dialysis is to give you the nearest experience to real kidney cleaning. He prefers 5-6 treatments a wk but will allow some to go 4 if they don't skip 2 consecutive days. He said the most ER visits and deaths of renal patients occur after weekends when patients haven't had regular cleaning and fluid removal.”
“5 days a week, it is about getting maximum cleaning of the blood.”
“Seems a shame to get home then limit yourself to virtually the same treatment as in centre.”
In a minimalist decorating philosophy and some religions, “less is more” is a way of life: Keep things simple; avoid clutter. But, when it comes to replacing continuous function of a vital organ with an intermittent therapy, less is less and more is more. In the U.S., we deliver minimalistic dialysis to most people who use standard in-center hemodialysis (HD; and some who use home HD)—and we have the distressing survival statistics to prove it.
Connect the Dots for Your Patients •-•-•-•-•
To me, questions like these from patients suggest that we need to educate them better about the big picture. Sure, we hammer on the vital importance of watching fluid, potassium, and sodium intake. But, we are clearly not successfully tying in information about frequency and duration of hemodialysis to patients’ quality of life, hospitalization rates, and survival. (If Dr. John Agar hadn’t retired, he would surely be banging his head against the wall right about now.). To help get you started, here are some things you can share with your patients.
Seven Key Points About HD Frequency
Before chronic dialysis began in the U.S. in 1960*, everyone with chronic kidney failure died.
Dialysis was scarce, costly, and “experimental.” Insurance did not pay for it. The U.S. Veteran’s Administration (VA) got temporary funding through federal grants to test dialysis.
Life and Death Committees” in Seattle (the birthplace of chronic HD) had citizens and clergy read charts of those who needed dialysis and choose whom to treat. Those who weren’t chosen died.
In 1960, people dialyzed once every 5-7 days when they felt ill.1 But, when they started to develop severe high blood pressure and nerve damage, Seattle switched to twice a week, then three times a week treatments.1
The three times a week HD treatment schedule is a historical accident. Since 4, 5, or 6 days a week HD was not tried, the Medicare ESRD Program chose three times a week HD when it began to cover dialysis in 1973.
Just three HD treatments in seven days means there has to be a 2-day gap. Bleyer et al analyzed day-of-week patterns of 375,482 deaths in the USRDS (1977 – 1997).2 Their findings? Sudden and cardiac death rates in HD patients were 45% higher on Mondays and Tuesdays—after the 2-day, no-treatment gap. This suggests that, at the very least, every other day HD would be better.
In 2010, the (badly flawed) Frequent Hemodialysis Network trials assigned 125 patients to do HD 6 days a week in-center, and 120 to do 3 days a week. A year later, the 6-day a week group had less risk of death or heart damage.3 More frequent HD removes less water at a time, so it can be more gentle than standard HD. That’s important! But, which matters more, HD frequency or session length? Read on: the answer may surprise you.
Five Key Points About HD Session Length
Let’s pop back to 1960 in Seattle for a moment. Those 2-3 times a week treatments were 8-12 hours long.1
Medicare never said how long treatments must be. Technically, blood in the lines = a treatment. Quality measures prevent that—but treatments did get much, much shorter: 15-18 hours/week in the 1970s, 12-15 hours/week in the early ‘80s to 6 to 12 hours/week in the late ‘80s.4 Ironically, the drop to 12 hours/week was partially achieved by raising dialysate sodium, while a further drop to 9 hours/week—with cranked up blood flow rates to maintain Kt/V—came after the results of the National Cooperative Dialysis Study.5
The National Cooperative Dialysis Study
Highly touted as a randomized, controlled trial, the NCDS in the early 1980s included just 151 patients ages 18-70—in four groups: short (2.5-3.5 hours) vs. long (4.5-5 hours) treatment time and high vs. low the time-averaged concentration (TAC) BUN concentration. After one year, the study found significant effects of BUN, but not time.6 Subsequent analyses led to the choice of Kt/Vurea as a measure of dialysis “adequacy,” with discussions about which equation was best going on well into the 1990s.
Interestingly, Dr. Tom Parker, an NCDS investigator and thought leader, jumped ship in 1994, noting: “There may indeed be a critical amount of time that is necessary in individual patients to achieve optimal ultrafiltration and blood pressure control. There may also be a critical amount of time necessary to achieve optimal solute removal.” 4
The importance of middle molecules was seen by 1972.7 These take membrane contact time to remove. Dr. Bernard Charra from Tassin, France where HD was done for 5-8 hours—and mortality was half the U.S. rate at the time—noted that “Among treatment-related factors, urea Kt/V has no significant effect on mortality, whereas the more time-related middle molecule index has a significant effect.”8
More costly high flux dialyzers came out in the late 1970s and sold as so much more efficient that treatment times could be shorter.9 One author boasted in 1984, “this approach permits drastic reduction of treatment time over conventional hemodialysis without sacrificing treatment adequacy.”10 The drop in treatment time? From 4 hours per session to just 2. NOTE: Less chair time was seemingly happy news for patients who could spend less time at the clinic and clinics, who could treat more patients per chair per day—until the dark side of this practice rather rapidly emerged…
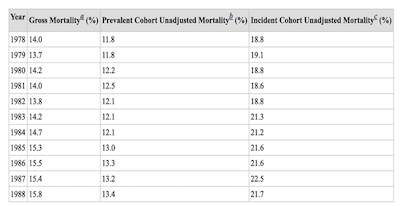
HD mortality rates in the U.S., rose by 13% in 1983 (the early high flux days…). The dangers of short HD sessions and benefits of longer ones began to be noticed:
Marshall et al published an analysis of 4,193 adult incident three times a week HD patients for whom they had data. HD sessions of 4.5-4.9 hours had the lowest death risk.11
In a Dialysis Outcomes and Practice Patterns Study (DOPPS) paper (one of my all-time favorites), Dr. Rajiv Saran et al found that every extra 30 minutes of HD time was linked with a 7% lower relative risk of death.12
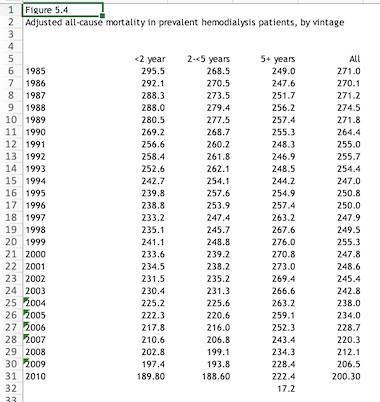
A second DOPPS analysis found the shortest average HD treatment time (TT) in the U.S., at 214 minutes, with Australia-New Zealand the longest, at 256 minutes.13 As before, mortality risk was lower for patients with longer TT.
In analysis of data from 2,382 people on HD, Dr. Jenny Flythe found 26% higher all-cause mortality when TT was less than 4 hours—regardless of patient age, gender, and dialysis weight.14
Which Matters Most, HD Frequency or Treatment Time?

This question has been asked over the years, and, of course (as you no doubt suspected), both matter. But, one really may matter more, and it may not be the one you think.
We don’t have randomized, controlled trials (RCTs) here. Due to their cost, there are only a handful of large, well-conducted RCTs in dialysis. In this case, the most recent large study uses data from the Australia and New Zealand Dialysis and Transplant Registry.15 Survival by HD treatment frequency and time were compared for all patients over age 18 who were not indigenous from 2001 to 2015.
A total of 16,944 patients were compared, of whom 757 received more than 3 HD sessions per week and 518 did treatments longer than 5 hours. After controlling for frequency, those who did 5+ hour HD treatments had a significantly lower risk of death than those who did 5 hours or less. The risk of death for more than 3 sessions per week was about the same as it was for 3 sessions. So, there is our answer: time seems to matter more than frequency.
Conclusion
Arming patients with the information they need to advocate for safe treatments requires that we learn our own history and share it with them. More dialysis is more likely to lead to full, rewarding, and active lives.
Blagg CR. The early history of dialysis for chronic renal failure in the United States: the view from Seattle. Am J Kidney Dis. 2007 Mar;49(3):482-96↩︎
Bleyer AJ, Russell GB, Satko SG. Sudden and cardiac death rates in hemodialysis patients. Kidney Int. 1999 Apr;55(4):1553-9↩︎
The FHN Trial Group. In-center hemodialysis six times per week versus three times per week. N Engl J Med. 2010 Dec 9;363(24):2287-300↩︎
Parker TF. Role of dialysis dose on morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 1994 Dec;24(6):981-9↩︎
Port FK, Morgenstern H, Bieber BA, Karaboyas A, McCullough KP, Tentori F, Pisoni RL, Robinson BM. Understanding associations of hemodialysis practices with clinical and patient-reported outcomes: examples from the DOPPS. Nephrol Dial Transplant. 2017 Apr 1;32(suppl 2):ii106-ii112↩︎
Lowrie EG, Laird NM, Parker TF, Sargent JA. Effect of the hemodialysis prescription on patient morbidity. Report from the National Cooperative Dialysis Study. N Engl J Med. 1981 Nov 12; 305:1176-81↩︎
Kramer P, Matthaei D, Go JG, Winckler K, Scheler F. Effect of blood factor deposits in reused dialyzers on the dialysance of middle weight molecules. Proc Eur Dial Transplant Assoc. 1972:9:278-89↩︎
Charra B, Laurent G, Chazot C, Jean G, Terrat JC, Vanel T. Hemodialysis trends in time, 1989 to 1998, independent of dose and outcome. Am J Kidney Dis. 1998 Dec;32(6; Suppl 4):S63-70↩︎
Mion C, Beau MC, Deschodt G, Gullberg CA, Ramperez P, Shaldon S. Reduction of treatment time with high flux postdilutional hemofiltration (HF). Proc Clin Dial Transplant Forum. 1979:9:63-5↩︎
Von Albertini B, Miller JH, Gardner PW, Shinaberger JH. High-flux hemodiafiltration: under six hours/week treatment. Trans Am Soc Artif Intern Organs. 1984:30:227-31↩︎
Marshall MR, Byrne BG, Kerr PG, McDonald SP. Associations of hemodialysis dose and session length with mortality risk in Australian and New Zealand patients. Kidney Int. 2006 Apr;69(7):1229-36↩︎
Saran R, Bragg-Gresham J, Levin NW, Twardowski ZJ, Wizemann V, Saito A, Kimata N, Gillespie BW, Combe C, Bommer J, Akiba T, Mapes DL, Port FK. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the DOPPS. Kidney Int. 2006 Apr;69(7):1222-8↩︎
Tentori F, Zhang J, Li Y, Karaboyas A, Kerr P, Saran R, Bommer J, Port F, Akiba T, Pisoni R, Robinson B. Longer dialysis session length is associated with better intermediate outcomes and survival among patients on in-center three times per week hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2012 Nov;27(11):4180-8↩︎
Flythe JE, Curhan GC, Brunelli SM. Shorter length dialysis sessions are associated with increased mortality, independent of body weight. Kidney Int. 2013 Jan;83(1):104-13↩︎
Emmett CJ, Macintyre K, Kitsos A, McKercher CM, Jose M, Bettiol S. Independent effect of haemodialysis session frequency and duration on survival in non-indigenous Australians on haemodialysis. Nephrology (Carlton). 2020 Apr;25(4):323-31↩︎


Comments
Dori Schatell
Sep 23, 2024 2:31 PM
Nancy Verdin
Sep 19, 2024 8:44 PM