Back to the Unit - A {Very} Temporary Change

Dialysis, or for me home dialysis, just sort of chugs along normally. The routine is familiar and, if I’m honest, quite comforting. I’m generally well, and my routine is well set. I’ve been on home hemo for close on 6 years. Dialysis is now just the final chore of the day: I lock the doors, clean my teeth, and do dialysis.
For over 4 years I’ve been doing my hemo overnight while I sleep, 8 ½ or 9 hour sessions at a time. It’s theoretically every other night, so Mon, Wed, Fri and Sun one week and Tue, Thur and Sat the next week. But, in reality, I often do back-to-back nights (e.g., Fri and then Sat) to change the off-days in the coming week to make the treatment schedule fit into my life better.
This means I average
over 30 hours of dialysis each week and often get more than 36
hours; three times the 12 hours typically given in centre here
in the UK. This means I live largely unaffected by issues like fluid and
diet restrictions that typically affect the lives of many dialysis
patients. And, as a result, I’m well and don’t really
think of myself as a “patient” at all.
And, as a result, I’m well and don’t really
think of myself as a “patient” at all.
Throwing a Wrench into the Works
On 24 September, though, that familiar routine was interrupted. Doing some DIY I had an accident and tore my bicep muscle, so I could no longer perform my own dialysis. I had no other option but to return to in-centre care with all that entails—12 hours of treatment, fluid restriction, and a need to be mindful again of food intake and how it affects things like potassium and phosphate.
I’d done dialysis over Sunday night as normal, missed Monday as planned, then couldn’t manage dialysis on Tuesday evening because of the injury. So, heading into Wednesday, the urgency of the need for some blood cleaning was creeping up. My nurse, Kate, managed to get me in a hospital for urgent treatment Wednesday afternoon and then for a Tue, Thur, Sat slot in a unit closer to my home for as long as I needed it.
As a result of watching webinars like this one by Dr. John Agar and other reading and learning, I have a self -imposed limit for fluid removal ([ultrafiltration] UF rate). Ordinarily, I won’t go higher than 400ml/hour. Over 8.5 hours, that limit allows me 3.4 litres of fluid to be removed. If I have a little more fluid, I would do a longer treatment, say an extra half hour, and remove up to 3.6 litres. Or, I would do another night’s treatment back-to-back, which gives me 17 hours or a maximum 6.8 litres to remove slowly and safely over the 2 nights.
Striving for Safe, Gentle In-centre HD
I’m well aware that anything above 600ml/hour UF rate leaves me absolutely exhausted after dialysis, but with only 12 hours of treatment scheduled, I had to compromise. So, I agreed to remove 2.4 litres of fluid over the 4 hours, a UF rate of 600 ml/hour and I increased my blood pump speed from the 220 I use overnight to 300 ml/min.
By the weekend (just 5 days after my last nocturnal treatment) with just 12 hours of dialysis completed and the prospect of another potentially harmful 3 day gap in treatment, I was already beginning to feel the effects of fluid building up inside me and the increased toxic load from the solutes I’d been unable to remove from my system because of the (for me) lack of time on dialysis.
I remembered EXACTLY why I’d chosen home dialysis and why after 2 years at home I’d switched to nocturnal: 12 hours of dialysis felt BRUTAL to me! It was taking SO MUCH out of me! I was napping both during and after treatment and snacking much more than usual. Oh, and the fluid! My obsession with fluid was back, as I tried—without any success at all—to limit myself to the mere 500 ml of fluid that would keep my fluid gain down to acceptable levels in the period between dialysis sessions.
Home HD to the Rescue
I cracked. We had the dialysis machine sat there doing nothing and an increasing need to get closer to normal treatment levels—so, between my wife and I, we managed a system-relieving additional treatment over the weekend, avoiding that 2-day gap, bringing the toxic load down, and removing an additional 2.4 litres of the fluid that was starting to build up.
Five sessions into my new in centre routine, because of the relentless march of time and the calendar clicking over into October, the monthly blood tests were done—and they don’t make for good reading. Less than 2 weeks away from my nocturnal home hemo routine and everything that is normally great looks troubling and everything that is normally in the “attention” zone has shot into a “needs action” area (see lab reports below). The standard response to this would be more medication and more restrictions. I’d be put back on phosphate binders with these results for sure! I’ve also gained exactly 2kg in the 2 weeks. It’s most probably a litre per week of fluid, because of the double whammy struggle with fluid restriction/refusal to raise UF beyond 600/ml/hour. But, it could also be some real weight because of the extra snacking and lack of movement during daytime dialysis when I would normally be mobile.
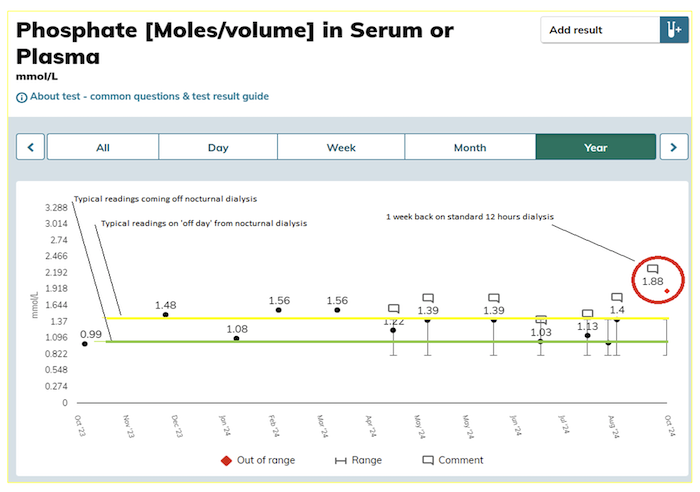
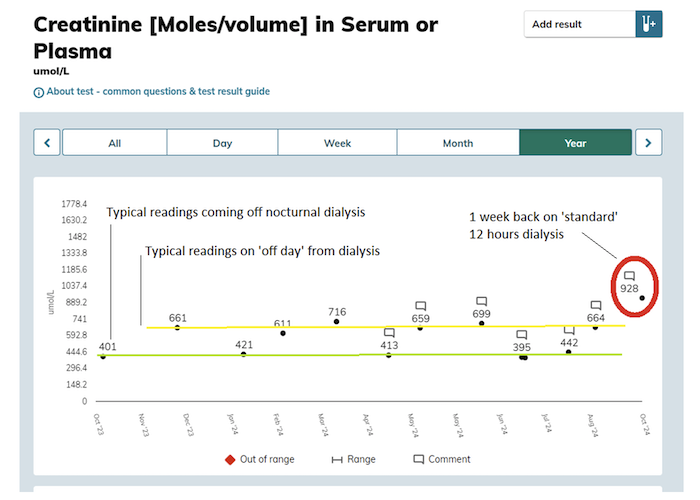
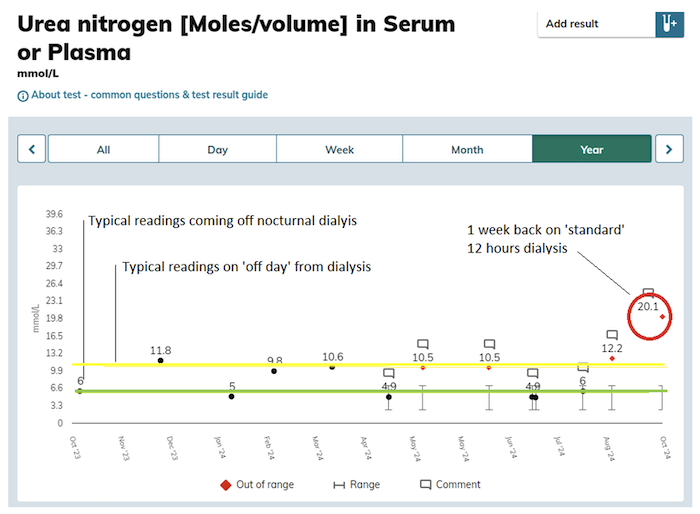
Fortunately for me, I’ve got a far greater range of motion in my arm now, enough for me to safely resume home therapy and self-care. So, after just 6 sessions and 2 weeks of in centre treatment I’m heading back home where I can get the additional hours of gentle treatment I need to maintain both a low UF and enough hours of treatment to effectively clean these solutes/toxins from my system. Hopefully my next set of bloods will be back to normal—for me!



Comments
John Agar
Oct 31, 2024 12:41 PM