Daily Nocturnal Home HDF - 2 Year Update

Reprinted with permission from https://www.kamaldshah.com/2024/09/daily-nocturnal-home-hdf-2-year-update.html. Originally published on September 8, 2024.
It’s been a little over two years now since I switched to Daily Nocturnal Home HDF. Very few people around the world are on this modality. It was disconcerting at first to make this switch. There’s hardly any (no?) published literature around this modality. I switched because it seemed to be the logical thing to do given the clinical symptoms I was having. My nephrologist also egged me on. And a nephrologist from the UK, Dr. Sandip Mitra had referred to it in one of his publications.
Two years hence, it seems I did the right thing. It was, by no means, an easy journey. There were pitfalls. I had to navigate my way around them with the help of my own nephrologist, the brilliant Dr. Rajasekhara Chakravarthi and getting tips from Dr. Mitra from time to time given the experience he had in dealing with patients on this therapy.
I blogged about my experience after 1 month, 3 months, 6 months and 1 year already.
At the end of two years, here are some of the challenges I faced and how I overcame them.
Yo-yoing Beta-2 Microglobulin
The main reason I switched to this modality was that my Beta-2 Microglobulin (Beta-2m) was rising continuously and causing symptoms such as shoulder pain at night and Carpal Tunnel Syndrome. HDF is known to help with Dialysis-related Amyloidosis, a well-established effect of increased levels of Beta-2m.
While my Beta-2m did go down in the beginning, it started rising in August 2023. And then suddenly fell around December of that year. And then started rising again in May 2024. Every time the levels started rising, my holder pains would return. Perplexing! However, I recently cracked this puzzle. Well, at least I like to think so.
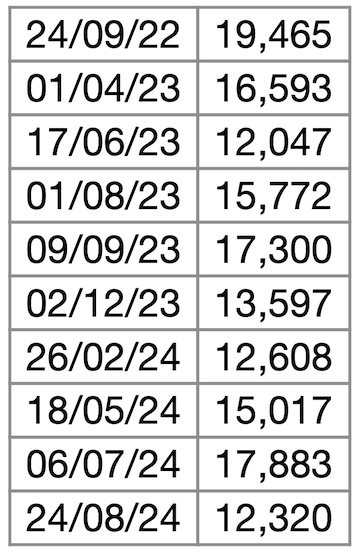
Here’s a table of my Beta-2m variations over the last two years.
What I realised was that the quality of water is paramount in HDF. While I did have a two-stage RO plant for my dialysis, there was no way for me to know whether the levels of Endotoxins were being met as per the requirements for HDF. I could not find any labs in India where they test endotoxins to the level required for ultra pure water required for HDF which was less than 0.03 EU/ml. The labs tested only up to levels of 0.25 EU/ml.
Coincidentally, a few months after the levels started rising after falling initially, the RO manufacturer changed the membrane during the course of some routine maintenance. A few weeks after, I checked my Beta-2m. It fell! I did not correlate the two at at time though.
Recently, again, my Beta-2 m started rising and the shoulder pains reappeared. I went over the timeline of this happening the last time and realised that the levels started falling soon after the RO overhaul. So, I asked the manufacturer to change the membranes and the loop line as well. Lo and behold my levels started falling recently!
So, lesson learned was to ensure the RO plant is maintained well and the parts are changed as needed. Trouble is in dialysis centres such as those managed by NephroPlus, there is a team that takes care of these things and there is strong oversight. At my home though, everything is on me. And life happens. I forget to check. I overlook. But I will be more vigilant going forward.
Yo-yoing iPTH
I have had quite a tempestuous relationship with iPTH. It is like a capricious beast that rears its head whenever it chooses. Without any logic. Without any rationale. And gives me bone pain. I managed to reach some semblance of stability by experimenting with various combination of calcitriol, cinacalcet, dialysate Calcium and dialysate Phosphate, and reached a steady state. Just then, I decided to move to HDF. Suddenly, this equation was not valid any longer because HDF works very differently compared to HD.
My iPTH started falling and reached dangerously low levels even when I was not on any calcimemetics. Why was the iPTH falling then? I figured it must be the HDF. But what could be done?
One solution could be to use a low Calcium bath for my HDF. I checked with the supplier. He said he could make it specially for me. I was relieved. I was using a 3.5 mEq/L Part A can. I requested 2.5 mEq/L cans. He supplied them to me. I tried it for a week and then tested my iPTH, Calcium and Phosphorus. It had swung the other way. The iPTH shot up and the Calcium went too low. I then started mixing the two cans in a 70-30 ratio to yield a 3.2 mEq/L Calcium solution. With that the iPTH is where I would like it to be. And so is the Calcium.
Phosphorus
Most dialysis patients have high Phosphorus levels. Ever since I switched to daily nocturnal home HD, I have had severely low Phosphorus levels. I started adding a Phosphate solution to the Part A can. With this, my Phosphorus reached respectable levels. However, when I switched to Daily Nocturnal Home HDF, I stopped adding the Phosphate solution as it was not sterile and in HDF, the dialysate mixes with the blood. I switched to an oral Phosphate supplement. With that, though the Phosphorus levels were good, I needed to be aware that the Phosphorus levels were probably falling to very low levels during my night session and then coming to normal after I took the supplements in the morning. But I left it at that.
Recently, though, the oral Phosphorus supplement started giving me a little diarrhoea. I thought the ideal thing to do was to add the Phosphate solution. I checked with Dr. Mitra of the UK and he said they do that in the UK for nocturnal HDF patients and recommended that I do that as well. I started adding it to the Part A cans. I was a little nervous due to the non-sterile nature of the solution. I kept a vial each of Avil and Hydrosortisone handy just in case I had a pyrogenic reaction. Thankfully, it was all fine. My Phosphorus levels are also fine now.
Summary
Overall, I am happy I switched to this modality. It gives me much better clearance of Beta-2m and probably a host of other middle molecules which we are not even aware of. I am also grateful to be able to afford this therapy and have access to be able to do it at home. This also goes to show that with kidney failure, the patient has to be in the driving seat. We have to be proactive about our health. Read up all you can. Have discussions with your doctor. Identify your goals from treatment and together with your doctor, arrive at solutions to achieve those goals.


Comments
LEONG SENG CHEN
Nov 07, 2024 9:31 PM