Alport’s Syndrome and My Life

When you are 62, a thumbnail
sketch of your life is on a freakishly large thumb. I inherited
kidney problems from my mom, who carried Alport Syndrome.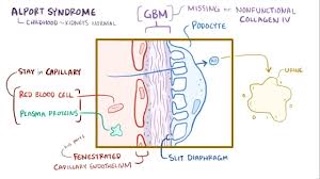 In my
family all the boys were affected, the first being Tony, who got sick
and died in 1971 at age 16. My one living brother has had a transplant
or been on dialysis since June of 1973, 32 years on transplants and 19
years on hemodialysis. He is a comedy writer, living in New Jersey, and
we talk daily and consult with one another about emerging health issues
we have experienced over the years.
In my
family all the boys were affected, the first being Tony, who got sick
and died in 1971 at age 16. My one living brother has had a transplant
or been on dialysis since June of 1973, 32 years on transplants and 19
years on hemodialysis. He is a comedy writer, living in New Jersey, and
we talk daily and consult with one another about emerging health issues
we have experienced over the years.
A biopsy in 1972, just before my 10th birthday, confirmed my own Alport’s diagnosis. Because of the family history, I saw a nephrologist every few years as a kid, and every year after I turned 16. My BP began to rise in 1982, and the doc prescribed a beta blocker. I worked full-time as a corporate security guard and maintained my medical insurance through my employer so I would be prepared when my kidneys weakened. I also attended college part-time for the better part of 9 years and I finished my B.A. in Psychology in 1989.
After 6 years of increasing meds and climbing creatinine, I started PD in April of 1988. PD was great because it allowed me the independence to continue working and going to college and to do my fluid exchanges on my schedule. I was able to travel widely and simply had my supplies shipped to where I would be staying.

Getting and Losing a Transplant
I did PD for almost 2 years then received a cadaveric transplant in March of 1990. Beginning in 1991, I worked as a software trainer for brokers, traders and other financial professionals, first for Quotron, then Reuters America. I got married in 1991 and my daughter, Sarah, was born in 1993. Unfortunately, the marriage ended in divorce in 1999.
The years from 2000 to 2002 were tough, as the transplant slowly stopped working and ultimately failed in November, 2002. I went back on PD, this time with a cycler for another 2 years. From July 2004 and for the next 4 months on the cycler I didn’t clear toxins well, gained fluid weight, and even the 4.25% dextrose bags were not pulling much, just keeping up. I was diagnosed with an umbilicus hernia at the end of 2004, had a chest catheter installed in January of 2005 and began hemo in-center.
Starting to Support Others

In July of 2005, I moved from New York to Cleveland to help my dad around the house and save on expenses while I paid down medical debt. In September 2006, I started a support group in Brook Park, OH that met in a local library conference room. The group is still running with monthly meetings, on Zoom since COVID hit. We meet on the 2nd Thursday of each month from 7:00-8:30 Eastern time. Interested? email me at ecoaker@sbcglobal.net for more information.
I met another patient, Jenna, and we began dating in 2012 and married in 2018. Sadly, she had a good deal of heart trouble over the years and succumbed after a 4th heart attack in April, 2022. Her grown daughter, Laren, still lives with me. She is my care partner.
Until this October, I had been at the same center since 2005. I switched to in-center nocturnal when it was offered in February 2010 and began self-cannulating with buttonhole needles to preserve my fistula and minimize aneurysms.
Transitioning to Home Hemo with NxStage

I had been considering home hemo from the time NxStage became available, and had one of their reps give a talk about NxStage to my support group in 2015. I was happy with my nocturnal modality, had excellent results, and felt mostly normal with 21 hours of weekly dialysis. I began to talk to people who did home dialysis and we compared notes.
As I compared in-center nocturnal to home hemodialysis, the main advantages for HHD seemed to be more freedom to travel and being able to set my own hours. I was living well and enjoying my days.
Then came COVID-19. Staffing issues closed the nocturnal shift at my unit in August, 2021, but my unit was able to accommodate the nocturnal patients’ prescriptions on an afternoon/evening shift. I was still happy doing long treatments 3 times each week, despite not having all my afternoons free. Further staffing crunches came this Spring, and our last 7 and 8-hour shifts were shut down on Friday, April 12th, 2024—a date that will live in infamy, at least with me.
I began to dialyze for just 4 hours three times a week and immediately felt the difference. My blood flow had been 300 for 7 hours and became 375 for 4 hours. After that schedule change I began to plan for home hemo with NxStage. I had to do a lot of organizing and cleanup in my house, as my late wife, her daughter, and I are all collectors, so we had a lot of things to re-home and organizing to do.
Finally, in September, I contacted NxStage for orientation. My NxStage training lasted from 14 October until November 25th. The last 3 days were with a nurse at home, on the same machine I would be using at home. The training was thorough and well-planned. I was told to forget about in-center; that this was a completely different animal.
What it’s Like to Bring Hemo Home
My prescription was quite different and there are safeguards to improve my experience and simplify the process. For example, less heparin is needed, due to the closed circuit of tubing that includes the dialyzer. The best part of the NxStage Versi HD with GuideMe software is the GuideMe aspect. The machine’s touchscreen shows me step-by-step how to go about setting up and getting on the machine, and deal with Caution alerts and Alarms. It reinforced my memory at every turn, building my confidence quickly.
I was ready to go home a week earlier but there was a delay when I was surprised to find my room had no grounded outlets. A previous owner of my 65-year-old house had installed 3 prong outlets, but there was no ground wire. A retired electrician friend was kind enough to help me install a new circuit on short notice, despite his busy schedule preparing to visit family down south for the winter.
My first NxStage delivery came on November 5th with PAKs and SAKs and cartridges, drain tubing and hanging bags and tubing. My ancillary supplies arrived on the 10th and the BioMed installer brought the NxStage Versi HD machine to my house on the 18th. I went home with the nurse that Thursday and my first true solo was on Tuesday the 26th. My prescription is currently 3 hours, 5 days each week, with blood flow set at 300 ml/minute.

My ultimate goal is to do 6 or 7 hours of nocturnal for 5 or 6 days and get the kind of clearance that requires no binders and affords me a diet very similar to what I could eat on my transplant in its prime. Isn’t it all about feeling normal whatever that is for you? Jenna always said, “‘Normal’ is a cycle on a washing machine and means different things to everyone.”
I did my first solo at home treatment with the NxStage Versi HD machine, using the SAK last Tuesday and last Thursday was my first solo with hanging bags. I even gave myself 50mg of Venofer. All has gone well. I have had a few alarms, but nothing I wasn't trained to handle. Laren is my care partner, but I am listed as solo, so she's really more of a butler. I thought about calling her Jeeves if she was okay with that. “There will be no Jeeves,” she said. It turns out that her sense of humor is not quite the same as mine…
With dialysis, longer treatments are better for my heart, I seldom feel toxic, treating on more days also eases the fluid burden on my vascular system, and I feel stronger and more alert, with fewer side effects. Kidneys work 24/7, but dialysis is MY job.


Comments