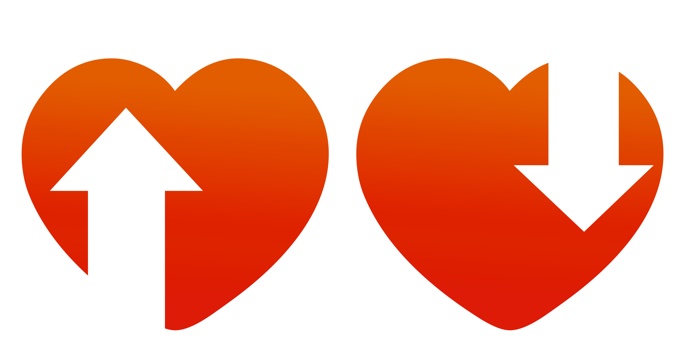
Rethinking AVF Needling Techniques - (Make both “pointy ends” face towards the heart!)
More than a decade ago, Zyblut Twardowski asked me if I would be prepared to challenge the audience (ADC: Tampa 2004) on the myths and legends surrounding needling techniques for native arteriovenous fistulae (AVF).
He and I shared a similar view – one first put forward in 1974 by Woodson and Shapiro (Dialysis and Transplantation: 1974) (1) – that:
- Routine use of retrograde arterial cannulation to avert recirculation is, in fact, based on a myth.
- Recirculation—if or when it occurs—is not the result of the direction (“antegrade” or “retrograde”) in which the needle is inserted, but is a reflection of a mechanical failure in the AVF
- Routine use of retrograde insertion for the arterial needle had no scientific basis but, rather, grew out of the ‘historical’ practices of the early shunt days where the arterial limb of the shunt had to be faced into the flow-direction of blood; there was no other option . But…when the AVF took over as the preferred access, a similar ‘into-the-flow-of-blood’ insertion practice continued.
- The propensity for arterial site aneurysm formation and fistula macro-distortion may be directly as a result of this practice.
- The “adequacy” of dialysis…if I dare use that abhorrent term…has nothing at all to do with needle direction and/or recirculation, but is purely and simply a function of (1) dialysis duration, (2) dialysis frequency, and (3) access patency and function. The rest is window-dressing—if that!
Woodson and Shapiro’s report in D&T (1974) showed some rare and elegant “footage” of fistula histology, a pictorial view of medicine we far too commonly ignore in the biochemically-driven world we now inhabit, that gives serious pause for thought.

Note the endothelial flap, the extravascular leakage, and the extra-luminal micro-false-aneurysm formation.
I have schematically depicted their hypothesis in the following few sketches:



Prove it for yourself. Take a 14 gauge fistula needle and some thick card, like the backing cardboard for a pad of paper, and try pushing the needle through it at a 45 degree angle. Then, carefully withdraw the needle. Hold up the card and look across the bottom of the card in a planar view. You will see a flap of cardboard poking down behind the insertion site…just like Woodson and Shapiro’s histological section and my schematics.
Now imagine the two opposing situations within the AVF after needle withdrawal:
(1) The needle is inserted in a retrograde direction…i.e., with the endothelial flap (the needle-hole ‘lid’) facing into the high velocity of ‘arterialised’ blood flow. Upon needle withdrawal, blood would be forced and guided into the tract left by the needle. Leaving the tract open and unsealed would thus cause, or at least potentiate, microscopic blood leakage into the perivascular tissues .
(2) The same needle is inserted in an antegrade direction… i.e., with the directional flow of blood. Upon needle withdrawal, the endothelial flap (or tract ‘lid’) inside the AVF would be forced flat and held “shut” by the force and directional flow of blood, closing the tract and preventing leakage .
In 2003, we presented our data to the ANZSN—later published as an abstract in Nephrology(2)—showing no change at all in PRU or KTV in 26 patients where “adequacy” was studied sequentially over 6 weeks under both needling orientations. There were no differences in “adequacy” data between the two insertion techniques.
In 2005, Harman(3) reported no difference in “adequacy” with either directional insertion technique though, in the same year, English (4) reported a small advantage to retrograde insertion.
In 2008, in a study similar to our own, 22 patients from Turkey were reported in Clinical Nephrology (2008) (5) … again this showed no difference in URR or eKt/V between retrograde or antegrade arterial puncture techniques.
Thus, from an “adequacy” perspective, it is clear that time, frequency and a healthy fistula are the key components and that needling orientation is highly unlikely to be of any clinical relevance at all.
We are thus primarily left with the question: does recurrent needling affect the structural integrity of the skin + subcutaneous tissue + vascular wall and, if so, which needling technique is least likely to damage this tri-layered interface between the circulation and the exterior?
To be honest, the right answer is: we don’t know! And, to think that we have done maintenance dialysis for 60+ years and still can’t answer that fundamental question is—I would argue—an indictment of us all.
The best available documentary evidence suggests that the main reason for using the retrograde insertion technique is based on a myth. It just doesn’t hold up. There is no dialysis advantage to continuing a retrograde arterial puncture technique. None.
However, the best available observational evidence suggests that aneurysmal damage is far more common at the arterial site, and that— while unproven—a common-sense assessment might conclude that recurrent extravascular leakage and wall-weakening through microaneurysmal formation from retrograde needling (á la Woodson and Shapiro) is a significant causal factor in the macro-structural changes we observe at the arterial site.
There is a great need for more work in this area as, without a doubt, the vascular access is still the key structural weak point in dialysis. And it is a weakness that, to our shame, we know little (if anything) more about now than when Woodson and Shapiro first questioned needling orientation more than 40 years ago.
In Australia and New Zealand, I am pleased to say that retrograde arterial puncture is now rare but, anecdotally, it is still practiced in places elsewhere.
If so, it is past time that that practice be reviewed … and changed.
References
- Woodson, R., & Shapiro, R. (1974). Antegrade vs Retrograde cannulation for percutaneous hemodialysis. Dialysis & Transplantation. p 29-30.
- Wiggins KJ*, Agar JWM, Somerville CA. A controlled study of the impact of arterial needle direction on dialysis adequacy in patients undergoing haemodialysis through a radio-cephalic arteriovenous fistula. (Abst.) Nephrology (Carlton). 8 (Suppl.), A70. August 2003.
- Harman E, The Arterial Needle can be placed in the direction of flow to achieve effective treatment. ANNA 2005. 32 (2): 224–225.
- English D. Retrograde arterial needle placement improves dialysis adequacy. ANNA 2005, 32 (2): 224.
- Ozmen S, Kadiroglu AK, Ozmen CA, Danis R, Sit D, Akin D, Yilmaz ME. Does the direction of arterial needle in AV fistula cannulation affect dialysis adequacy? Clin. Nephrol. (2008). 70(3): 229-32.


Comments
Henning Sondergaard
Nov 13, 2014 2:36 PM
The points that Woodson & Shapiro made then and that Dr.Agar is making now seem so much like common sense that it's astounding it should still be discussed. And it is downright scary that doctors have such a poor grasp of basic physics that they were/are not able to see it sooner.
It's just another sign of how dialysis has such low status amongst nephrologists. It boggles my mind how so many of them decide to study the ins and outs of some obscure kidney disease while largely ignoring how to better the outcomes of those affected by it - and by all the other causes of CKD.
And it is deplorable when we look at how many resources go into exploring every nook and cranny of the effects of transplantation while basic knowledge of dialysis, like agreeing on a measure for 'adequate dialysis' or 'what markers are important to look at' are easily put to the side or brushed off as 'less important'.
That's why we have to applaud the few doctors, like Dr. Agar, who put all their professional pride in working in the dialysis field. The question is thus, how do we get more of them to take an interest in this (very important) sub-field of nephrology?
It's not as if dialysis is about to disappear in any foreseeable future, after all.
George Harper
Nov 08, 2014 2:11 AM
George Harper
Rome, GA