What to Look for in a Home Dialysis Clinic
So, you've done your homework and you want to do dialysis at home. And you've chosen the type of treatment you want to do. But where? If you have more than one choice of home clinic, how do you decide which will be the best fit for you?
(Don't know which clinics near you offer home treatments? Look for them in our "Find a Clinic" database.)
Bigger is often better
A key question to ask a home program is, "How many people are doing my treatment choice at your clinic?" In home dialysis, bigger truly is better. It may seem that a program with 2 or 3 dialyzors might give you lots of personal attention. But in a small program, the home training nurse—your main contact—will likely be pulled between home and the in-center unit. The result: less time for you.
Successful programs say that each home training nurse can train and follow about 20 people. So, a program with 20 people on peritoneal dialysis (PD) or home hemodialysis (HD) may have a nurse just for home dialyzors. A program with 40 people will likely have two nurses—so they can take turns being on call, and can both answer questions.

Some programs have gone to a regional model instead of having lots of small programs. This is a bit more driving, but it's better for you.
Larger programs may have other pluses, too:
- Policies that evolved through trial and error may be more user-friendly for you
- More experience with the types of challenges you might run into
- More people doing your type of treatment who may be willing to talk with you
No large program in your area?
- Look in a wider area.
- A home dialysis clinic doesn't have to be right around the corner—it can be as far away as you are willing to drive once a month for clinic visits. We know of people who even moved to another city or state to get the type of treatment they wanted.
- Offer to be a peer mentor.
- You can help a smaller program grow by volunteering to talk to other people who are dialyzing in-center and might be interested in home dialysis. Ask your local paper or magazine to write a feature story about you. Talk at health fairs. Happy dialyzors are the best salespeople for home treatments.
Look for experienced staff
Another key question to ask a home program is, "What is the home dialysis background of the training nurse(s)?"
In the Conditions for Coverage (the Medicare rules that cover dialysis clinics) section 494.140(b)(2), it lists the experience a home training nurse must have:
Self-care and home dialysis training nurse. The nurse responsible for self-care and/or home care training must—
- Be a registered nurse; and
- Have at least 12 months experience in providing nursing care and an additional 3 months of experience in the specific modality for which the nurse will provide self-care training.

This level of nurse training is a minimum. If the only program in your area has staff who are new to home, ask what resources they have to help them answer tricky questions or solve challenges. Or, you may find yourself doing a lot of problem solving on your own or online.
Ask how many people the nurse has trained. A nurse who has trained only a handful of people may not be as helpful as someone who has trained a dozen or more. Ask to meet the person who will do your training, too—not just the program director. Be sure that you can work with the nurse who will train you.
How are home patients doing?
Sure, home treatments are work friendly. They may be easier to fit into your schedule. They can help you regain control of your life. But the reality is, you do end up with set-up and clean-up, supplies to order and track, treatment logs to keep and send in, and a fair amount of work to do.
The real benefit of home treatments is that you can feel better, have a more-normal diet, stay out of the hospital more—and even live longer. So, ask, "What are the clinical outcomes of people who are doing the type of treatment I want?"
If you plan to do PD, ask about infections. Good clinics may have just one infection per several years of PD. This means they're doing a great job with training—and of motivating people to do their PD with care.
If you plan to do home HD, ask the program what outcomes they are tracking and how people are doing. If they can answer you, it's a good sign that they are paying attention. The data they collect can also help to prove that home HD is a better, safer treatment option than standard in-center care.
Will you choose me?
Programs differ in their beliefs about who is best suited to do a home treatment. This means, "How will you decide if I can do home treatment at your clinic?" You may get a different answer based on where you go.
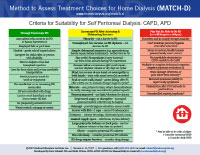
We encourage clinics to use our Method to Assess Treatment Choices for Home Dialysis (MATCH-D) 1 tool. This tool helps clinics assess people for home treatments and overcome any challenges they might have.
We believe the best predictor of home dialysis success is how motivated you are to do your treatments at home. A clinic that would turn you down because you are a minority, older, a single parent, can't hear well, etc., may not be one you'd want to go to anyway. If a clinic turns you down for home treatment and you know you can do it, look for another clinic.
Do-it-yourself hemodialysis
A home program's philosophy of care has a lot to do with how much you vs. a partner—will do on home HD. Research has found that when a dialyzor does more (and the partner, if there is one, does less), success is more likely. 2,3,4 So, ask the program, "How much of my treatment do you expect me to do, vs. a partner?"

A clinic that says, "we'll teach you to do as much as you can," has your best interest at heart. A clinic that trains your partner to be your tech—while you sit as "the patient"—may be setting you both up to fail.
Many partners find putting in dialysis needles to be very stressful. Placing your own needles may make you more likely to succeed in the long-term. If you truly can't do it (i.e., you don't have the use of one hand), be sure to thank your partner for making it possible for you to be home.
Some programs don't require a partner—but may require a Lifeline button device that can call 911 or someone who can reach you quickly if you hit a snag.
If you are quite ill when you start home HD, you may not feel well enough at first to take on a lot of your own care. When you start to feel better, take some of the burden off of your partner by doing what you can by yourself. And be sure to say "thank you" for what your partner does for you. Showing appreciation can mean a lot.
Talk to me about training
- "How long will it take me to get a training slot?"
- If you have a good job with a health plan, and want to keep it, this is a key question. You may be better off seeking out a clinic that can get you in sooner rather than waiting months and taking the chance of losing your job. (You can do in-center treatments while you wait, but you may not feel well enough to work—or the time slot you get may not fit with your job.)
- "What will my training schedule be?"
- Ask to see the training plan, and find out what a typical day will be like. What will you learn, when? How long might it take? Can it be done around your work day?
- "Will my care partner (if I have one) and I train alone, or with others?"
- Some clinics are training 2-4 people (and partners if they have them) in small groups. This can be a way to shorten waiting lists and create a built-in support group for dialyzors and partners. If your learning styles are very different, having someone else there could push you faster than you'd like or slow you down. Whether you prefer one-on-one or group training is a personal decision, but it's something you'll want to ask about.
Home sweet home visits

"Will you do a home visit when I start doing my treatments by myself?" Many—if not most—programs will do a home visit before you start home training, to see how your home can be set up to make things easier for you. A home visit can help you figure out the best place to set up your machine or store supplies—or how to have pets and do home treatments safely. But the first treatment at home on your own is still stressful. Your nurse may visit for your first treatment to ease your transition. Whether you do PD or home HD, a home visit can help you start off on the right foot.
Even after you get started, some programs will do a home visit to be sure that you have what you need, and to help you troubleshoot if you run into a problem.
Don't be a dropout!
"What percentage of your home patients go back to in-center treatment?" Most home dialyzors feel much better. But treatment at home may not involve just you—it can throw a wrench into your home life if you are not ready for it. Each year, as many as 30-40% of people who start home treatments decide to quit—most in the stressful first 3 months.
Some programs do a better job than others of supporting both patients and partners (when present)—and they have very low dropout rates.
The difference? They make sure that you know exactly what to expect, and who will do which tasks. They take their time during training so you feel confident that you can handle things—and even bring you back in for a refresher if you need it. They call you to see how you're doing and if you have questions you haven't gotten a chance to ask. They focus on making your life work for you (not on making you fit into their structure).
Conclusion
Home dialysis can improve your life—and choosing a good clinic can make your home treatment experience better.
Checklist
- How many people are doing my treatment choice at your clinic?
- What is the home dialysis background of the training nurse(s)?
- What are the clinical outcomes of people who are doing the type of treatment I want?
- How will you decide if I can do home treatment at your clinic?
- How much of my treatment do you expect me to do, vs. a partner?
- How long will it take me to get a training slot?
- Will my care partner (if I have one) and I train alone, or with others?
- Will you do a home visit when I start doing my treatments by myself?
- What percentage of your home patients go back to in-center treatment?
References:
- Method to Assess Treatment Choices for Home Dialysis (MATCH-D). Home Dialysis Central.
- Atcherson E. Home hemodialysis and the spouse assistant. J Am Assoc Nephrol Nurses Tech. 1981; 8:29-34.
- Marshall JR, Rice DG, O'Mera M, Shelp WD. Characteristics of couples with poor outcome in dialysis home training. J Chron Dis. 1975; 28:375-381.
- Streltzer J, Finkelstein F, Feigenbaum H, Kitsen J, Cohn GL. The spouse's role in home hemodialysis. Arch Gen Psychiatry. 1976; 33:55-58.

