View from the Chair: Balancing Burdens and Benefits Between Home and In-Center Dialysis

Eons ago it seems—in 2005—I wrote an article (just a page; really a blog precursor!) for the Nephrology Nursing Journal.1 My point was that virtually the entire renal community assumed that in-center hemodialysis (HD) treatments were the least burdensome because, “You leave the driving to us.” But, this perspective ignored the heavy burden of in-center HD on family roles, work life, spontaneous travel, emotional stress, strict diet and fluid limits, etc. Home treatments have burdens, too—but different ones, like needing to order supplies, set up the machine, cannulate, tape, monitor, document, and clean up... Now that a new article suggests adding an assessment of treatment burden to inform patient choices,2 it seemed like time to revisit the balancing act between the burdens and benefits of home vs. in-center dialysis by asking those who know best—people who have used two or more different dialysis options—to rate each one on a scale of 1-10, where 10 is the highest burden.
What quickly arose in the conversation that followed was the notion that it makes very little sense to consider burdens without also asking whether the associated benefits make the burdens worthwhile. As one respondent explained: “I was talking to my husband about this. He said the burden score for PD is 4, and in-center HD is 4. He prefers PD by a million, and his comment was ‘if she wants a burden score, maybe she would also like a score on how you feel after dialysis—how comfortable you are, how much freedom you have with diet, and how safe you feel while doing dialysis. His point was he would rather spend 30 times the amount of work to ensure he gets the best quality of care and freedoms.”
Another noted that:
“For me, any burden like managing supplies, setting up and taking down my PD cycler each day, etc., is a manageable burden. I always feel better and more stable with daily treatments and other benefits have always outweighed any inconvenience of PD.”
This made me think of a Teeter Totter or balance scale, with benefits on one side and burdens on the other. Several people were specific about exactly what constituted burdens vs. benefits for them. Each individual’s values help to frame what is a burden and whether the burdens are outweighed by benefits.
Several people found PD to have the fewest burdens and greatest benefits:
“9 years on PD, 4 years on home HD, and 3 years in-center. I like PD the best because it is fairly easy to travel with and I had no trouble sleeping with it. Home HD is almost as good, but travel is more difficult. In-center was the worst: I felt bad all the time, was sick a lot more, and I had to drive to center on their schedule.”
“Cycler PD overnight is by far the best! Maybe not lab report-wise, but energy and functionality for sure! I have done PD, in-center HD, now home HD. I can tell you just from MY opinion, PD!
“Respective scores: 10 - in-center, 7 - home HD, 4 - PD. Time on dialysis, comorbidities, age, etc. will have an impact on subjective burden, which will vary from person to person. To me, burden is a combination of psychological factors and the purely physical, including the practicalities of carrying out the treatment. Added into that are other psychosocial factors that make people’s lives meaningful, be it work, family, hobbies, travel, etc. I tend to lump PD together, but I have done CAPD, PD with a cycler, in-unit HD, short daily HD, and nocturnal home HD. It makes more sense to me to simply assign most burdensome to least, while trying to consider all the factors that come into play. So, here we go:
 In-unit HD
In-unit HDShort daily HD
Nocturnal HD (a bit of a tie with short daily, but the burdens are different)
CAPD
PD with a cycler”
“I did a few months in a center on HD using a permacath. It sucked. I then started PD. I liked it. The only burden was the boxes of fluid, and peritonitis sucks—I had it three times in 15 years. I had an upper arm fistula made and while I was waiting for it to mature, had another permacath. I’ve been doing home HD for 8 years. I had a short time when my aluminum level went sky high and I switched to hanging bags, which was better, but again had a lot of boxes and had to hang eight bags per treatment. I recently extended treatment time to 5 ½ hours 5 days a week, so I can run a slower blood flow rate (easier for my heart) and went back to making dialysis fluid via the PureFlow. PD was my favorite mode of treatment.
A number of respondents preferred home HD. One did not feel burdened at all by this choice, while another looked at dialysis as another job. Two felt quite burdened—but still felt that the benefits made their efforts worthwhile, particularly because they valued autonomy and control. Several felt that home HD was less burdensome than other options they’d tried:
“Home HD is a burden 1—not a burden for me at all! I actually look forward to my treatments, and I feel great. Four days a week, I am solo, and hours 2 ½.”
“I do NxStage now, for almost 4 years. I get up at 5:30 and set the machine up, then we go out for breakfast and come back and do treatment. I try to just look at it as another job I now have. I was always up early. I do go through phases where I feel like it’s a burden, but it keeps me here and I’m in my own home. Did the center for 2 months at the beginning and that was nothing but a burden. It would literally tie your whole day up.”
“I’ve done in-center HD and home HD with NxStage. I’d rate the burden of in-center around 4 or 5, the main burden being getting to and from treatment. Home HD rates a far higher burden score for me. Some days, like today when I’m traveling and had issues with treatment last night, I’d give home HD a burden score of 10. On less stressful days, I’d still give home HD a burden score of 8. That doesn’t mean I don’t prefer home HD—it is far better for me, but it also requires much more from me. The biggest way home HD is better for me is in allowing me to schedule it when it works for me. I recover faster from treatment, but that was never a major issue for me. It also means I don’t have to get out on winter roads three times a week.

“I’d rate my burden score much higher for home HD. Sometimes the work that goes into home HD gets glossed over, even here. I don’t think it makes my life any easier, it’s just a different kind of hard. I do feel better, not much, but some. I have no desire to return to in-center, but I do try to be honest about the work involved. Home HD is enough better than in-center that I’d consider Hospice if I were forced back in-center. And, I really did pretty well in-center. Being in charge of my treatment makes a huge difference for me.”
“In-center 10, home HD with CVC: 5, home HD with fistula: 2. I gave the 2 because stress of the unknown plays heavily on my mind and my ability to react and resolve ‘first time’ events remains questionable. Also, home with a CVC meant many more supplies—heparin injections, higher risk of infection (I was obsessed with sterile fields, so we were fortunate to manage for 5 months without any issues), and the CVC process is more detailed and significantly longer in time.”
“I would rate in-center a 7. I had morning treatments Mondays, Wednesdays, and Fridays and getting up in the morning and driving to the center was difficult for me. Also, being in the center was depressing for me, and I hated sitting in that chair for 4 hours. I felt very drained. The thirst during the weekends was unmanageable and I could not take it. I would rate home HD a 3, because of the difficulty traveling. The machine with the travel case is about 100 pounds. I live alone and always have to ask somebody to help me with the machine from my home to the Uber car, from the Uber car to the airport check-in, from my arrival at the airport to the rental car service, then from the rental car to my hotel. I get airport carts, however I still need help lifting the machine off the cart to the van or rental car or hotel room. If the machine was at least 50 pounds lighter, I would give the difficulty a 1.”
“PD – 8, for us, because it ended up with a 4-day hospital stay to drain liquid from around the lungs. Just didn’t work. The peritoneal lining leaked within 8 hours. Center – 10. Husband hated this and has said if he had to go back would most likely just stop. Huge burden to him as you have to go when a chair is open, their schedule, dealing with techs who act as if they are life itself, and not helping you live a full life but are there to keep you alive. Home HD – 4: keep supplies organized, set up hook up and take off. The low burden is about poor quality of life being taken away and feeling better, energy, and being able to live a normal life outweigh all else. Doing nocturnal gives more free time all week. The burden of doing dialysis can be mental as much as time consuming. With in-center, the mental roadblock for the next treatment would start the minute he stepped out of the clinic. Hell, I would tote 20 boxes up 5 flights of stairs not to have him go through that.
“Hubby enjoyed all the friendships made in-center (patients and nurses) but felt like pure crap after every treatment. He almost died from peritonitis on PD and says he will never do PD again. Two transplants (one living, one deceased) gave him a break from dialysis, but transplants have their own set of issues and side effects. Home HD (NxStage 4 days a week for about 3 hours) is—by far—hubby’s #1 choice of dialysis. It’s a lot of responsibility (almost like a part-time job for him and for me), but there’s also a lot of flexibility and independence. He feels MUCH better on home HD and has better labs. Travel is difficult but doable. As a caregiver, I prefer home HD for hubby, too. He has been deemed “ineligible” for a 3rd transplant. He started dialysis when he was 39 (he will soon be 63). We are very lucky and live a good life.”
“I have done in-center HD, PD, and home HD. In-center would be 10 for most of a burden. I felt worse only doing dialysis 3x a week. Didn’t feel well after treatment and commuting home was awful. PD would be a 5, moderately burdensome. I am not a good sleeper, so being stuck in my room for 10 hours a night was not ideal. I also did not like storing all of the supplies, and got peritonitis when they had to switch my PD catheter to the other side. Home HD would be the least burdensome for me at a 2. The supplies are minimal and I feel much better with less restrictions dialyzing 5x a week. My runs are only a little over 2 hours.* I get tired of making SAKs every 3 days, but it is better than lifting heavy bags.”
*NOTE: Five treatments of “a little over 2 hours” a week equal fewer than 12 hours of HD per week—less than most in-center dialyzors get. More hours of HD do a better job of removing middle molecules, but, of course, also add to the burden of treatment…
Finally, one individual felt he’d been misled about the benefits of home HD compared to the burdens—his life worked better when he did in-center treatments.
“In-center was a 4 or 5. Home HD is an 11. While in-center, I was able to work over 40 hours a week. I just had to get there and they did all the rest. I’m now doing home HD alone at my house, and I’m not able to work anymore, because I have four treatments a week for 5 hours at a time, because the machines aren’t as thorough as the center machines. I have to set up everything, do needles, etc. I was told it would make my life easier and it hasn’t. The one good thing is I can do it whatever time of the day I need without a schedule. But, it’s a lot of work. You still need to meet with nurses, draw labs and FedEx them, schedule supplies…”
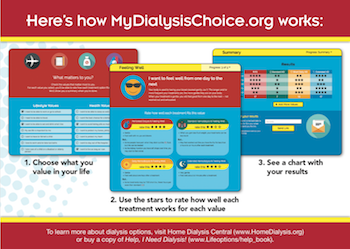
This is an important point—and one that illustrates why a benefits vs. burdens approach—really just a riff on the old “pros and cons”—is not enough. What matters most to someone? If keeping a job is what matters, short daily HD is often not the best fit, because it takes so much time out of a day that is already full. PD or nocturnal HD in-center or at home are better fits for working folks. Values-based treatment matching is why we built My Life, My Dialysis Choice.
Finally, I leave you with the perspective of a 20+ year dialyzor whose positive attitude has no doubt contributed to his long-term success: “I prefer to focus on what is best, not worst. It’s more about life, and how to be able to find normality—not go looking for burdens.”


Comments
Lloyd Tiegs
Nov 04, 2018 5:06 AM
Dori
Nov 05, 2018 8:04 PM
George Said
Nov 01, 2018 10:29 PM
I have had PD, I have had Hospital HD and now home HD. In each case Dialysis has kept me alive. What is there to complain? I have happily dealt with my circumstances.
Dori
Nov 02, 2018 1:51 PM