A Sea Change in Nephrology Training for Home Dialysis

Greater adoption of home dialysis—both peritoneal dialysis (PD) and home hemodialysis (HD) has had a number of system challenges, including nephrologist training. In 2007, Dr. Todd Ing told me he founded the International Society for Hemodialysis (ISHD) because only about 10 of the 140 or so U.S. nephrology fellowship training programs required a hands-on rotation in chronic hemodialysis. Most fellows saw dialysis patients only in the ICU—so, likely few could imagine patients doing their own treatments at home. Simultaneously, the American Board of Internal Medicine (ABIM) nephrology certification exam “blueprint” had just a dozen questions on any type of dialysis—5% of 240 items. Together, this was a perfect storm: training programs knew fellows could easily pass the exam without knowing any dialysis.
In 2010, when we conducted a 13-item national, fax-back survey of nephrologists (n=629), we found that 38% of respondents did not feel well-prepared to care for dialysis patients at the point of taking the certification exam, and just 16% had obtained post-fellowship dialysis training.1 Not surprisingly, while 92% of U.S. patients received in-center hemodialysis (HD) at the time, only 6% of the nephrologists said they would choose this option if their own kidneys failed and they had a 5-year wait for a transplant. Instead, 45% would have chosen peritoneal dialysis (PD), 25% would have opted for daily home HD, 18% for nocturnal home HD, and 3% for in-center nocturnal HD. The bright spot? “Nephrologists practicing for <10 years were significantly more likely to treat patients with daily, thrice weekly, nocturnal home HD, or nocturnal in-center HD than nephrologists practicing for +11 years (p< 0.02).”
thrice weekly, nocturnal home HD, or nocturnal in-center HD than nephrologists practicing for +11 years (p< 0.02).”
Today, both of those nephrologist training dynamics have changed: we are en route back to a future that embraces home therapies.
Advocates had been pushing for change. In a 2012 editorial, Dr. Robert S. Brown2 asserted that just one year of dedicated clinical experience—with ½ day per week in the second year—was insufficient, proposing more case-based patient teaching time. He noted that a passing score on the ABIM exam requires only about 60% correct answers (75% of items are case-vignettes). By requiring all fellows to have “dedicated nonclinical research time,” the Accreditation Council for Graduate Medical Education (ACGME) detracts from training time for those who plan clinical careers. The ASN In-Training Exam, aimed at improving ABIM exam passage rates, resulted in just a 5% improvement rate in case-vignette questions over the 2 year training.
Dr. Jeff Berns et al agreed, citing a need to identify core skills for all nephrologists,3 and noting that in a 2010 survey (by Berns), nearly 20% of 133 respondents did not feel competent to care for in-center HD patients, 45% did not feel competent with PD—and 84% with home HD. The authors recommended that “minimum experience with each dialysis modality should be explicitly defined, as well as the level of skill needed in caring for patients treated with each modality.”
Fellows themselves, meanwhile, wanted more instruction in home dialysis modalities, with 45% of 320 respondents in a 2017 survey desiring to learn more about PD, and 51% about home HD.4 Only 55% of second-year fellows felt “fully prepared” for independent practice.
 In 2019, release of the Executive Order creating the Advancing American Kidney Health Initiative (AAKHI) shone a spotlight on home dialysis, galvanizing the industry (A global COVID-19 pandemic has further shown the benefits of keeping people safely in their own homes, rather than subject them to several hours, thrice weekly, of sitting with a mask on during treatment to avoid infection.) Just prior to announcement of the AAKHI, the ACGME released new, 2019 nephrology fellowship requirements. The phrase “dedicated nonclinical research time” no longer appears, and there is a considerable amount of specificity around dialysis training. This includes (bold emphasis is mine):
In 2019, release of the Executive Order creating the Advancing American Kidney Health Initiative (AAKHI) shone a spotlight on home dialysis, galvanizing the industry (A global COVID-19 pandemic has further shown the benefits of keeping people safely in their own homes, rather than subject them to several hours, thrice weekly, of sitting with a mask on during treatment to avoid infection.) Just prior to announcement of the AAKHI, the ACGME released new, 2019 nephrology fellowship requirements. The phrase “dedicated nonclinical research time” no longer appears, and there is a considerable amount of specificity around dialysis training. This includes (bold emphasis is mine):
I.D.1.d).(5): The program must provide acute and chronic hemodialysis, continuous renal replacement therapy, peritoneal dialysis, and renal biopsy. (core)
I.D.4.a).(1).(a): The program should be of sufficient size to ensure fellows’ adequate exposure to patients with…chronic dialysis both hemodialysis and peritoneal dialysis including patients who utilize home dialysis treatment modalities, in order to ensure adequate education and experience in chronic dialysis. (Detail)
IV.B.1.b).(2).(b): Fellows must demonstrate competence in the performance of the following procedures: (i): acute and chronic hemodialysis (iv): peritoneal dialysis. (core)
IV.B.1.c).(3): Fellows must demonstrate knowledge of (b): Dialysis and extracorporeal therapy, including (core) (b).(i): the indication for each mode of dialysis; (b).(iv): kinetic principles of hemodialysis and peritoneal dialysis; (b).(v): the principles of dialysis access… (b).(vi): the short- and long-term complications of each mode of dialysis and its management; (b).(vii): the artificial membranes used in hemodialysis and biocompatibility; and (b).(viii): urea kinetics and protein catabolic rate.
IV.B.1.c)(3). (core) (n): The principles and practice of hemodialysis and peritoneal dialysis; (o): the technology of hemodialysis and peritoneal dialysis; (q): the psychosocial and ethical issues of dialysis.
IV.C.3 A minimum of 12 months must be devoted to clinical experience. (core)
IV.C.3.a) Fellows should have at least four months of experience with dialysis therapies, both hemodialysis and peritoneal dialysis.(Detail)
IV.C.6 Clinical experience must include supervised involvement in dialysis therapy(core)
Beth Witten pointed out to me that The ABIM has a new, January 2020 “blueprint,” for nephrology certification—which is what prompted me to write this post. When Dr. Richard J. Baron took over leadership of the ABIM in 2013, he was at the CMS Innovation Center immediately prior, and happened to head up a section that my husband worked in at the time. So, I gave my husband our nephrologist survey paper to give to him. Did he read it? Did it matter? Beats me, but I tried! Compared to the blueprint I downloaded in 2008, there is considerably more emphasis on CKD (which includes ESRD)—and transplant (see table below)—which together now total 33% of the exam, compared to the previous 24%. Dialysis is included in questions for:
-
Hyperkalemia
-
Initiation and discontinuation of maintenance dialysis,
-
End-stage renal disease
-
Hemodialysis and peritoneal dialysis complications,
-
Treatment for ingestion of toxic substances, and ICU treatments
|
2008 ABIM Nephrology Blueprint |
2020 ABIM Nephrology Blueprint |
||
|
Content Category |
% of Exam |
Content Category |
% of Exam |
|
Chronic kidney disease |
14% |
Chronic kidney disease |
22% |
|
Glomerular/vascular disorders |
12% |
Glomerular/vascular disorders |
12% |
|
Kidney transplantation |
10% |
Kidney transplantation |
11% |
|
Hypertension |
10% |
Hypertension |
10% |
|
Sodium/water |
10% |
Sodium/water |
8% |
|
Acid-base/Potassium |
10% |
Acid-base/Potassium |
9% |
|
Clinical pharmacology & misc. |
10% |
Pharmacology |
5% |
|
Tubular/interstitial, cystic dz |
6% |
Tubular/interstitial, cystic disorders |
4% |
|
Mineral metabolism |
8% |
Calcium, Phosphorus, Mg, Stones |
4% |
|
Acute renal failure/ICU |
10% |
AKI/ICU nephrology |
15% |
|
Total |
100% |
100% |
|
Buoyed by this finding, I decided to delve into the list of fellowship training programs themselves. ASN currently lists 199 total programs (155 adult, 44 pediatric) in its directory. Several are closed or no longer offer nephrology, leaving 149 adult nephrology training programs. I looked at each program’s website to see whether PD or home HD were mentioned—and searched for them (where a search box permitted) if they were not. What I found (see pie chart) suggests that the tides have already turned, and a sea change is well underway. For clinical nephrologists, at least, it is now much more possible to choose a program that offers experience with home treatments.
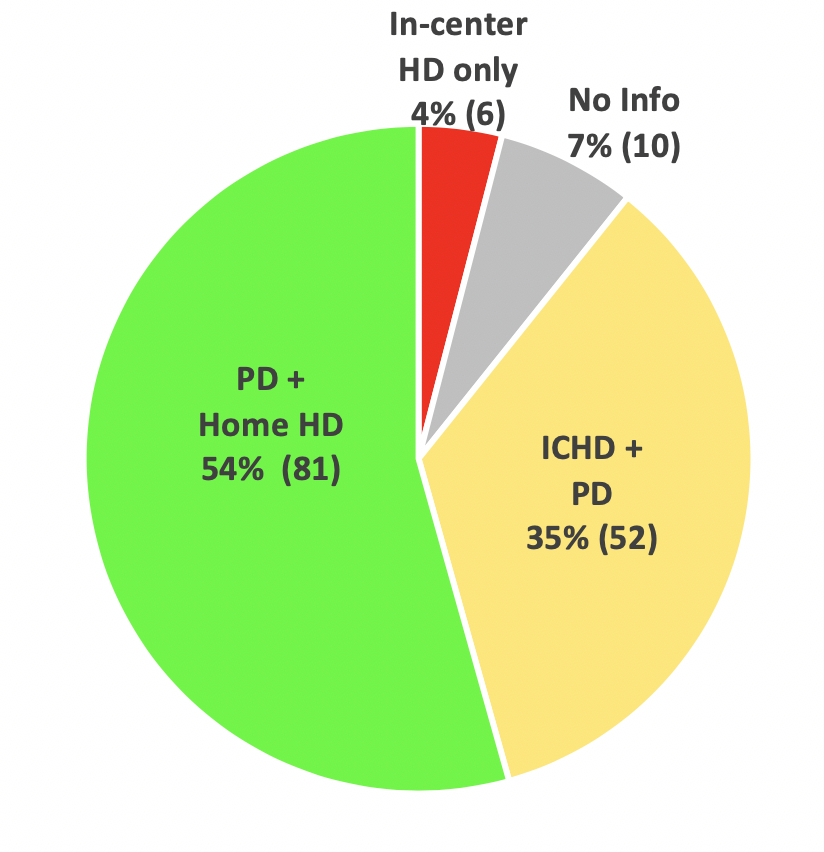
I did see some red flags: one program’s exposure of fellows to PD consisted of a one-day “PD University.” This is a great program—but not enough, I suspect, to make nephrologists fully comfortable with prescribing and managing PD patients and their complications. (Other programs may do this as well, but not mention it…) More importantly, I was surprised by a number of programs that did not offer home HD—but in some cases did research that affected it, such as Wake Forest. My quick research may have missed some options, though. If anyone is interested in the specifics of which program offers which options, please leave a comment with your email address—I am happy to share my data with anyone who would like to do a deeper dive, perhaps contact the programs directly, and publish the results.
1 Merighi JR, Schatell DR, Bragg-Gresham JL, Witten B, Mehrotra R. Insights into nephrologist training, clinical practice, and dialysis choice. Hemodial Int. 2012 Apr;16(2):242-51. Doi: 10.1111/j.1542-4758.2011.00648.x.
2 Brown RS. Is nephrology fellowship training on the right track? Am J Kidney Dis. 2012 Sep;60(3):343-6. Doi.1053/j.ajkd.2012.04.016
3 Berns JS, Ellison DH, Linas SL, Rosner MH. Training the next generation’s nephrology workforce. Clin J Am Soc Nephrol. 2014 Sep 5;9(9):1639-44. Doi: 10.2215/CJN.00560114
4 Rope RW, Pivert KA, Parker MG, Sozio SM, Merell SB. Education in nephrology fellowship: a survey-based needs assessment. J Am Soc Nephrol. 2017 Jul;28(7):1983-1990. Doi: 10.1681/ASN.2016101061


Comments
Nieltje Gedney
Jun 19, 2020 10:13 PM
Dori
Jun 20, 2020 12:49 AM
Nicole Leonard
Jul 21, 2020 8:14 PM
Dori Schatell
Jul 21, 2020 8:31 PM