ESRD Treatment Choices Model 2021: Opportunities, Challenges, and Clinic List

January 1, 2021 began the first measurement year of the ESRD Treatment Choices Model, which aims to increase home dialysis and access to transplant. The Model is described in the Special Care Models Final Rule, and data will be collected on how many patients with Original Medicare do home dialysis each month of each year from January 1, 2021 through June 30, 2026; the Model will conclude on June 30, 2027. This post will examine dialysis clinics selected for the Model and challenges some clinics and their patients with Original Medicare may face.
 The Special Care Models Final Rule mandates that 30% of dialysis clinics must participate. The Model describes how payments to participating clinics for home dialysis and services related to it will be adjusted up or down based on adoption of home dialysis. The CMS Innovation Center (CMMI) published the selected geographic areas—but not a list of dialysis clinics. Instead, CMMI provided a PDF and an Excel document listing 13,424 ZIP Codes.
The Special Care Models Final Rule mandates that 30% of dialysis clinics must participate. The Model describes how payments to participating clinics for home dialysis and services related to it will be adjusted up or down based on adoption of home dialysis. The CMS Innovation Center (CMMI) published the selected geographic areas—but not a list of dialysis clinics. Instead, CMMI provided a PDF and an Excel document listing 13,424 ZIP Codes.
Dialysis clinics were selected and mandated to take part in the ETC Model if they are located in 20% of the ZIP Codes in Maryland and in ZIP Codes in 30% of the 306 U.S.Hospital Referral Regions (HRRs). HRR boundaries must contain at least 120,000 people and can cross state lines.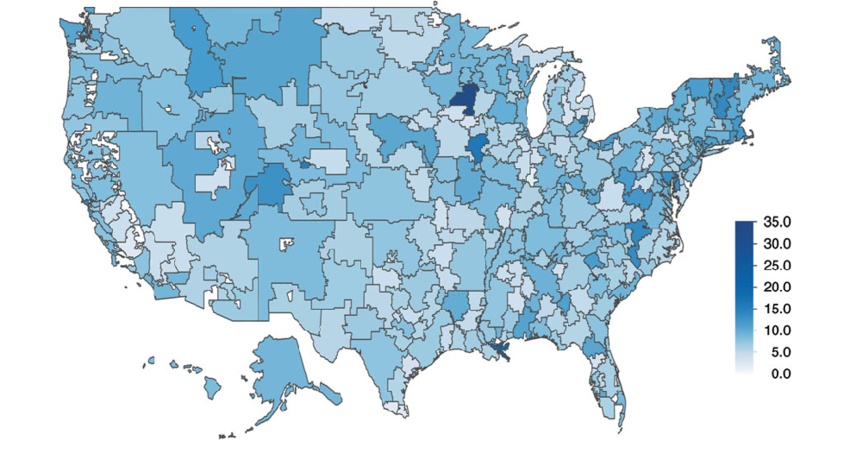
Kristi Klicko, the Medical Education Institute (MEI) Director of Operations, and I cross-referenced the CMMI’s ZIP Code list with the most recent data from CMS’ Dialysis Facility Compare (DFC) (9/2020) and ESRD Public Use File (PUF) (2/2020) to create a list of the dialysis clinics selected to take part in the ETC Model. You can download it from the Professional Tools page of Home Dialysis Central.
Of the almost 8,000 dialysis clinics in the U.S., we identified 2,432 selected for the ETC Model.
Of the 2,432 selected clinics:
-
1,187 clinics (49%) did NOT offer ANY home dialysis.
-
143 clinics were independents—not part of a multi-facility organization (dialysis chain).
— 58 of these clinics do NOT offer any home dialysis.
-
2,262 clinics are part of a dialysis chain.
— 1,129 of these do NOT offer any home dialysis.
NOTE: There are errors and discrepancies in both the DFC and PUF data we used for our analysis, including wrong ZIP Codes, clinic names, addresses, status of independent vs multi-facility, ownership, and treatments offered. Our analysis is based on the data available, and we made edits as we identified errors. In addition, some clinics may have started or stopped offering home dialysis since the data files were published by CMS. It is important for participating clinics to ensure that their data are accurate to assure appropriate home dialysis aggregation and payment adjustment.
Patient Involvement in the ETC Model Clinics
ETC patient notification is required for every dialysis clinic and Managing Clinician participating in the ETC Model. CMS has published a document with a flyer that provides this patient notification, with space for a clinic or Managing Clinician to add content. The current reading level of this flyer is a Flesch reading score of grade 15.59: far beyond the comprehension of many (likely most) patients. The flyer tells patients they are free to choose a provider and type of treatment. Changing clinics or Managing Clinicians would require the patient to find a clinic or Managing Clinician in a ZIP Code not in the Model. With the list we developed, you can help them by identifying a clinic that is NOT on the list and confirming that it is not in the ETC Model.
Patients are excluded from the ETC Model if they:
-
Do not have Medicare Part B
-
Are in a Medicare Advantage plan
-
Do not live in the U.S.
-
Are under 18 before the first date of service on the monthly claim
-
Have acute kidney injury
-
Were diagnosed with dementia
-
Live in a skilled nursing facility or nursing facility.
Financial Adjustments
-
The ESRD bundled payment will be subject to a Home Dialysis Payment Adjustment (HDPA) on home dialysis claims (Type of Bill 072X and condition codes 74 or 76).
-
Clinics with in-center self-care* (Type of Bill 072X and condition code 72) will get one-half the credit for home dialysis.
-
 Dialysis clinics will be subject to a Performance Payment Adjustment (PPA) based on the clinic’s rate of home dialysis from July 1, 2022 through June 30, 2027. The home dialysis rate will be aggregated across dialysis clinics under the same legal entity within the same HRR.
Dialysis clinics will be subject to a Performance Payment Adjustment (PPA) based on the clinic’s rate of home dialysis from July 1, 2022 through June 30, 2027. The home dialysis rate will be aggregated across dialysis clinics under the same legal entity within the same HRR. -
* CMS uses “self-dialysis” interchangeably with “self-care” and provides this definition: “Self-dialysis means dialysis performed with little or no professional assistance by an ESRD patient or caregiver who has completed an appropriate course of training as specified in §494.100(a) of this part (i.e., the Condition for Care at home in the ESRD Conditions for Coverage).
-
CMS Certification is required to offer home dialysis. A clinic can even be certified for home dialysis only. An existing clinic must request to add the service of home dialysis to its Medicare certification. Either way, a clinic must have the staff, training materials, and have trained at least one patient before it can be surveyed for approval for PD or home HD and subsequent Medicare payment. In-center self-care dialysis does not require separate certification—but, Medicare will only reimburse for in-center self-care training when a clinic is certified for home dialysis. A clinic with in-center self-care must provide patients similar training to that offered by home programs, with the expectation that in-center self-care patients will do all or most dialysis tasks independently.
-
Medicare will adjust Managing Clinicians’ payment based on how many of their dialysis patients are doing home dialysis (PD or home HD) and in-center self-care. Claims are identified with these CPT codes:
-
90957
-
90958
-
90959
-
90960
-
90961
-
90962
-
90965
-
90968
-
The Managing Clinician’s home dialysis rate will be aggregated across a group practice identified by its TIN and a solo practitioner’s NPI.
Challenges
The Final Rule states that chain-owned clinics in the same HRR can aggregate (combine) their home dialysis data. So, data for clinics in a chain that offer home dialysis can offset those that do not. This Rule can help clinics that don’t have home programs in multi-facility organizations to avoid some of the challenges independent clinics without home programs could face.

As we move forward, it will be interesting to see whether incentives in the ETC Model will encourage clinics without home programs to start new home programs—or whether clinics without home programs will at least start to offer in-center self-care. Some challenges to these efforts may be:
-
Space is needed for home dialysis as there must be at least one training room. PD does not require modifications, but home HD requires plumbing the training area.
-
Contracts will be required to provide home dialysis equipment and supplies and deliver them to patients’ homes where equipment is used by one patient only.
-
Staffing for home training requires an RN with 12 months of RN experience and 3 months in the type of dialysis s/he will be teaching. Fewer nurses have PD experience. Experienced nurses will come at a premium. Others will require temporary placement at a clinic where they can gain the 3-months experience. This may be easier for chains to provide than independent clinics.
-
Training materials must be user-friendly, which includes white space, steps in pictures, 6th grade reading level, etc. Independent clinics would need to start from scratch to develop these materials, while clinics within a chain can use training materials for PD or home HD developed by that chain.
-
Independent clinics and small chains without home programs may be vulnerable to takeovers if they may see cuts in their reimbursement due to not having home dialysis patients and not being able to aggregate data with other clinics that have home patients.
-
Patients in small new home programs may have staff with less experience in PD or home HD. A home training nurse’s inexperience could put patients’ home dialysis longevity at risk, if a frustrated nurse too quickly recommends that a patient return to in-center HD.
MEI Resources for Home Dialysis and Modality Choice
 MEI believe patients must be well-informed about home and self-care options. Dialysis staff and Managing Clinicians need to combat their personal biases and evaluate every patient for candidacy for peritoneal or home hemodialysis. MEI offers an array of easy to read FREE and low-cost tools to help dialysis clinics and Managing Clinicians.
MEI believe patients must be well-informed about home and self-care options. Dialysis staff and Managing Clinicians need to combat their personal biases and evaluate every patient for candidacy for peritoneal or home hemodialysis. MEI offers an array of easy to read FREE and low-cost tools to help dialysis clinics and Managing Clinicians.
-
My Life, My Dialysis Choice helps match treatment options to patients’ values and lifestyles.
-
 Home Dialysis Central has a wealth of information for patients and professionals about home dialysis options, including videos, patient profiles, tools, Life@Home articles, KidneyViews blogs, and more.
Home Dialysis Central has a wealth of information for patients and professionals about home dialysis options, including videos, patient profiles, tools, Life@Home articles, KidneyViews blogs, and more. -
The Method to Achieve Treatment Choices for Home Dialysis (MATCH-D) can help staff determine whom to encourage to do home dialysis, who might need to have barriers to home addressed, and who would need a care partner who does more to go home.
-
The Partner Agreement for Tasks for Home Dialysis (PATH-D) for PD and for HD is in English and Spanish and helps a patient and care partner divide tasks of home dialysis to keep the patient from feeling like a burden and the care partner being overwhelmed and burned out.
-
 Kidney School has modules to help patients understand home dialysis options and living with home dialysis, online, in print and as audio.
Kidney School has modules to help patients understand home dialysis options and living with home dialysis, online, in print and as audio. -
The Home Dialysis Central Discussion Group on Facebook is a members-only closed group where patients can ask questions and seek support from other patients and professional members.
-
The MEI Store has low cost or free items including post cards, bookmarks, books/booklets including Help, I Need Dialysis! as well as brochures, posters, UFR calculator, video with some items in Spanish.
Conclusion
The added incentives of the ETC Model give a shot in the arm to home therapies. These can now be added to existing incentives for home dialysis that:
-
Pay clinics the same for rate for home dialysis as for the higher labor and infrastructure costs of in-center.
-
Pay nephrologists 80% of the $500 allowed charge for each home trained patient.
-
Allow patients who start home training before the 4th full month the chance to get Medicare the month they start dialysis—instead of having a costly 3-month wait.
I hope the ETC Model achieves its goal of increasing utilization of home dialysis without making independent clinics lose money and become prey for chains, or having patients feel coerced to do a treatment a clinic or doctor wants them to do but they are not yet ready for. There have been a lot of positive articles published before the ETC Model was implemented, and we also need to be aware of the risks and prepare for the challenges. I hope this blog post has helped identify some of those.


Comments