Dialysis Staffing and Moral Injury: Patient Care vs. Policy

Dialysis care has been personal to me since I started in renal. I have several close friends who were affected by kidney disease young in life, and both my grandmother and step-father spent their last years of life on dialysis. When I took my first job in nephrology, I promised that I would treat the patients like family. I really did my best to follow through with that to the utmost of my capacity. I still am, from this vantagepoint.
As a working
dialysis nurse, the task of caring for people became
incomprehensibly more difficult for me on an ethical level the
more I learned about and came to understand the fundamentals. Early on
in my career, I was teased for being “book smart,” and took it with good
humor because it’s objectively a fair statement. I am, always have been.
I really enjoy going down rabbit-holes of information and connecting
dots in my head. It makes my brain happy, and this sort-of academic
furor runs in my family; it’s innate.
It makes my brain happy, and this sort-of academic
furor runs in my family; it’s innate.
Knowledge Comes at a Price
I was admittedly unprepared for the price: no one warned me. I spent my early days physically caring for patients, and many of the nights after at home on the couch, staying up late reading about how to do better for them. I had no idea that learning more would make the task of being a dialysis nurse easier in theory, but inexplicably harder in practice.
 MEI’s Home Dialysis
Central website changed both my career and my life. I remember
quite vividly first reading Dr. John Agar’s blog posts
about the
dangers of aggressive ultrafiltration, the harm caused by high
blood flow rates, and the
physiological implications of poor treatment. I recall these posts
well because I took my time really thinking about and trying to
visualize the entirety of those teachings. I then read all of his source
material! It got me into such a fury, I started Facebook-stalking Dori
Schatell and begging her for more information to devour.
MEI’s Home Dialysis
Central website changed both my career and my life. I remember
quite vividly first reading Dr. John Agar’s blog posts
about the
dangers of aggressive ultrafiltration, the harm caused by high
blood flow rates, and the
physiological implications of poor treatment. I recall these posts
well because I took my time really thinking about and trying to
visualize the entirety of those teachings. I then read all of his source
material! It got me into such a fury, I started Facebook-stalking Dori
Schatell and begging her for more information to devour.

I have still never met John Agar, but happen to know he is spending some of his retirement sending lovely Australian animal photos to my (now-boss) Dori. I’m delighted by this because I “heard” the frustration resonate in his writings a decade ago, and truly hope he is thinking about something else right now. Seriously, I hope he doesn’t even read this.
I empathize with John’s frustrations completely, and felt similarly towards the end of my clinical career. I’m poised to spend the rest of my life continuing the mission to educate America about inherent issues in our industry so that he can geek out over numbats for the rest of his. Seems like a fair trade for all of that knowledge I got for free on the Internet!
The education changed me, tangibly. It made me ask more questions, and examine the whole of my purpose and calling much more closely. The issues I struggled with predominantly surrounded areas where clinical practices and patient health uncomfortably intersect.
 How can a caring nurse reconcile
the ethical dilemma of knowing that an inappropriately high UFR
is absolutely doing permanent damage to a patient’s entire
body, while also following the policies that justify use of
those rates? If regulations say that 13mL/kg/hr is acceptable, why did I
find it so distressing to work in-center and have to program machines
for that? Was something wrong with me, or did I just know better? Book
smarts! The last thing I’d ever want to do is harm someone. The last
thing I’d want a nurse in my position to do is harm my loved ones who’ve
sat in those chairs, too. Once I saw this happening, I couldn’t
do it anymore.
How can a caring nurse reconcile
the ethical dilemma of knowing that an inappropriately high UFR
is absolutely doing permanent damage to a patient’s entire
body, while also following the policies that justify use of
those rates? If regulations say that 13mL/kg/hr is acceptable, why did I
find it so distressing to work in-center and have to program machines
for that? Was something wrong with me, or did I just know better? Book
smarts! The last thing I’d ever want to do is harm someone. The last
thing I’d want a nurse in my position to do is harm my loved ones who’ve
sat in those chairs, too. Once I saw this happening, I couldn’t
do it anymore.
Protecting Dialysis Access Sites
I happen to be fascinated by vascular access. As a nurse, I’ve never physically gone in and performed those beautifully delicate surgeries, but I carefully read about what goes on inside a fistula during a treatment long before I became proficient at cannulating them. I was able to see the turbulent blood-flow in my mind’s eye, and also the luminal damage that John Agar explained. Book smarts!
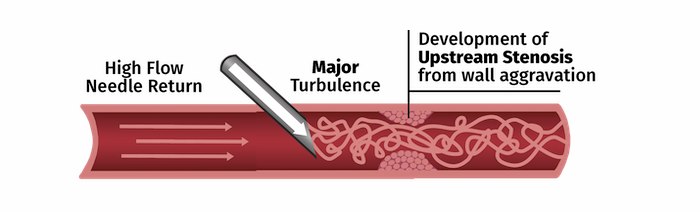 How
can a compassionate nurse reconcile the ethical dilemma of
having orders that call for a BFR of 500mL/min,
governing policies that support that practice, and the awareness that
rates over 400 cause harm? Once I understood, I couldn’t do it anymore.
Every time I saw blood flow rates set that high, I had to actively
resist the urge to lower the pump speed. It was unbearably
difficult to not interfere. I physically got to a point where I
couldn’t raise a BFR per orders for moral reasons. My loved ones and my
patients told me they felt terrible running at those speeds. That is
honest and valuable feedback.
How
can a compassionate nurse reconcile the ethical dilemma of
having orders that call for a BFR of 500mL/min,
governing policies that support that practice, and the awareness that
rates over 400 cause harm? Once I understood, I couldn’t do it anymore.
Every time I saw blood flow rates set that high, I had to actively
resist the urge to lower the pump speed. It was unbearably
difficult to not interfere. I physically got to a point where I
couldn’t raise a BFR per orders for moral reasons. My loved ones and my
patients told me they felt terrible running at those speeds. That is
honest and valuable feedback.
That level of understanding was hard to face on a daily basis. I have no idea how others who know these things cope; I found it exhausting and depressing. To continue, I had to work only in home therapies, where I could have some influence. I still struggled with the ethics of how patients are herded through the in-center units like cattle.
Putting Up the Ladder Against the Wrong Wall…
Kt/V is an industry staple that completely stressed me out once I gained the ability to critically think about it in-depth, too. “It’s not the K, it’s the t!” plays in a loop in my head—thanks for that, John! I had ethical debates with myself constantly over those “goals” because increasing time is physiologically best for the patient—but more burdensome to the clinic. Our industry mostly ignores the fact that this is really the underlying tone for how we are prescribing treatment. I don’t feel like that is ethical, but I do think it’s true.
Book smarts tell me that we don’t routinely test for BNP or B2M in the United States, even though those tests would give us much better ways to assess patients than the weak Kt/V. Yet, policies and governance paint Kt/V like it’s a be-all-end-all. It’s not. Dialysis is much more complex than that on a molecular level. A person can absolutely have a good-looking Kt/V and not be getting good treatment. Poor treatment usually leads to terrible quality of life and an agonizing death, too. No one wants that!
Moral Injury vs. “Burnout”
We have been in a seemingly downward spiral in healthcare for a very long time. We feel it in sub-specialties the most. It seems as though fewer nurses with my skill-sets are working in the clinical setting. Even fewer are teaching new nurses to do this work. The entire system is in a panic at every level. In some ways, it feels like a betrayal to have left my co-workers and patients during a “healthcare crisis” to move on to this job, where I have such privilege, working from home and getting to eat snacks and drink hot coffee at my desk…but one of the pitfalls of being an under-dog who truly enjoys learning is hitting a point where you can’t do anything with the information you hold anymore, because you’re up against a ceiling.

I know a lot of really brilliant nurses who left in “The Great Exodus” for similar reasons as I had to. It is called “burn-out” in healthcare, but the semantics of that phrase really imply that the fault is on the healthcare workers who are completely depleted from working in an industry that makes us ethically contradict ourselves constantly. There is a great YouTube video about moral injury made by Dr. Zubin Damania that I wish everyone would take a few minutes to watch. He says it far better than I can in this post. I firmly stand by every point he makes in the video, and if you’ve read this far—you probably will too. I encourage re-sharing.
In addition to the wise elders of nephrology who are retiring and moving on, how many eager, potentially rising, passionate newcomers are we losing due to the moral injuries caused by our education and practices being in opposition? How many more are suffering and still trying to hang-on when it feels impossible to provide the care they know the patients deserve? How can we pull the nose up on this plane, so that we can feel good about the care we give at the end of the day and it’s reconciled well with what we know to be true fundamentally?
 The system needs to change to
be sustainable. I can say that with clarity because I’m, at my core,
still a “frontline nurse” who works for the vulnerable humans who need
the strength of my voice most. I have felt the static between myself, my
patients, and the industry at large. It should surprise no one that
staffing issues are so prevalent. There really are great people working
in medicine, but also a great deal of distress as we try to
please diametrically opposed masters. This is the heart of the
elephant in the room.
The system needs to change to
be sustainable. I can say that with clarity because I’m, at my core,
still a “frontline nurse” who works for the vulnerable humans who need
the strength of my voice most. I have felt the static between myself, my
patients, and the industry at large. It should surprise no one that
staffing issues are so prevalent. There really are great people working
in medicine, but also a great deal of distress as we try to
please diametrically opposed masters. This is the heart of the
elephant in the room.


Comments
Henning Sondergaard
Apr 21, 2023 9:53 AM
Technologically, dialysis treatments haven’t changed since the 1960s - for 60 years, that is!! What other field of technical healthcare (or any other tech field for that matter) uses 60 year old technology? If the field of consumer electronics had followed that of dialysis machines, my phone would be 4 New York City blocks 40 stories high - trust me I’ve done the math. Why spend money on R&D when the meager competition also refrains from it, has been a question for at least 50 years in this business.
Also, the industry of providing treatment is not interested in keeping people alive, at least not if there is no ‘positive’ cost benefit for them. Provide enough chairs to get the zombies in and out as quickly as possible. They are not considered human beings anyway, because who would treat their fellow humans in such a way?
To me it’s not about pleasing two masters. It’s a matter of either making a living in the same way that WWII camp directors did while closing their eyes, or having enough compassion to say enough is enough. Nobody should be treated like cattle on the way to the slaughterhouse.
That’s what 11+ years of HHD and a multitude of blog posts, articles, talks, etc. has taught me. Have I been able to move anything? Not fundamentally. But like my dear friend, John A, would say maybe a few souls. Apparently, I can’t ask for much more. And like John I am getting incredibly tired of it - but unlike him, I can never retire from HHD without fatal consequences
Charlene Marie Vollmer
Apr 20, 2023 10:42 PM