ESRD Treatment Choices (ETC) Model: Year Two Update

History & Goals of ETC Model
When Medicare
started paying for dialysis in the 1970s, 40% of patients were
doing home dialysis. With Medicare payment there was a
mushrooming of dialysis clinics along with changes in patient
demographics that led to declining rates of home dialysis in the U.S.
that are now lower than in other developed countries. Rates of referrals
for kidney transplants have been low as well. To address these changes,
on July 10, 2019, President Trump issued the Executive
Order on Advancing American Kidney Health. Under Section 5 of the
EO, it said, “Greater rates of home dialysis and
transplantation will improve quality of life and care for patients who
require dialysis and may eliminate the need for dialysis altogether for
many patients.”
With Medicare payment there was a
mushrooming of dialysis clinics along with changes in patient
demographics that led to declining rates of home dialysis in the U.S.
that are now lower than in other developed countries. Rates of referrals
for kidney transplants have been low as well. To address these changes,
on July 10, 2019, President Trump issued the Executive
Order on Advancing American Kidney Health. Under Section 5 of the
EO, it said, “Greater rates of home dialysis and
transplantation will improve quality of life and care for patients who
require dialysis and may eliminate the need for dialysis altogether for
many patients.”
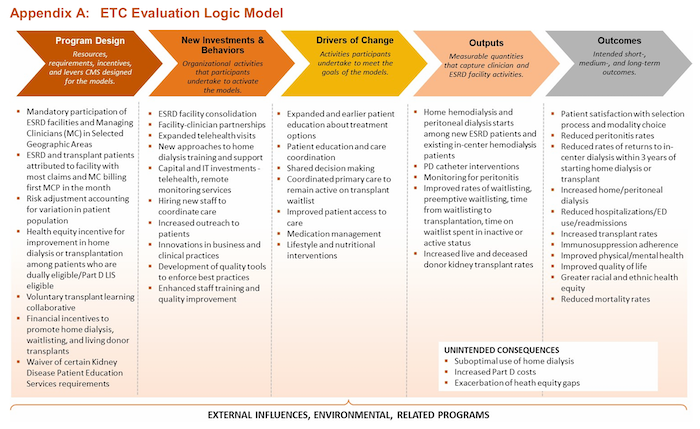
As the percentage of home dialysis patients declined, many expressed their concern that in-center hemodialysis has become the default treatment for people with kidney failure, including those who could be good candidates for home dialysis. At the same time, many patients on dialysis say they were not educated about treatment options. The EO charged CMS with choosing a model to increase the percentage of patients on home dialysis and with transplants. The CMS Center for Medicare & Medicaid Innovation (CMMI) developed a model it believed would incentivize dialysis clinics and managing clinicians to increase the percentage of patients on home dialysis and referred for transplant. The Department of Health & Human Services (DHHS) set an ambitious goal of 80% of new patients with kidney failure would be on home dialysis or have a kidney transplant by 2025. We are now midway through 2024.
The ETC Model’s Design
Participation in the ETC Model is not optional. More than 30% of dialysis clinics and Managing Clinicians (physicians and non-physician providers) located within certain Hospital Referral Regions (HRRs) in the U.S. were required to participate. Participating clinics had to meet certain targets and to increase the percentage of home patients to receive incentive payments. CMS granted clinics that offered in-center self-care and/or in-center nocturnal dialysis partial credit. Participating clinics owned by the same corporate entity were allowed to aggregate data, so clinics with no home program got credit for home dialysis rates at other clinics owned by that entity. Meanwhile, dialysis clinics that did not have a home program or that didn’t increase their home patient percentage after 2 years would be subject to negative adjustments. I wrote a blog in January, 2021 about the ETC model when it launched.
The First Annual Evaluation Report
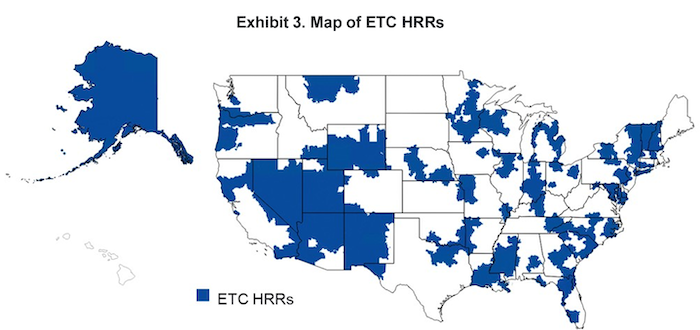
Because this blog is on Home Dialysis Central, I’m only going to update this blog with data on how the Model affected patients, clinics, and home dialysis outcomes. The Lewin Group, Inc. is a CMS contractor that is often called upon to evaluate CMS programs. In July 2023, the Lewin Group released The End-Stage Renal Disease Treatment Choices (ETC) Model, First Annual Evaluation Report. In the report, using qualitative and quantitative data, they “examined potential impacts of the model on several outcomes that include home dialysis use, transplantation, service utilization, Medicare payments, QoC, and patient experience of care.” The report included this map showing HRRs where participating clinics and Managing Clinicians were located.
Here's the breakdown of those required to participate in the ETC Model:
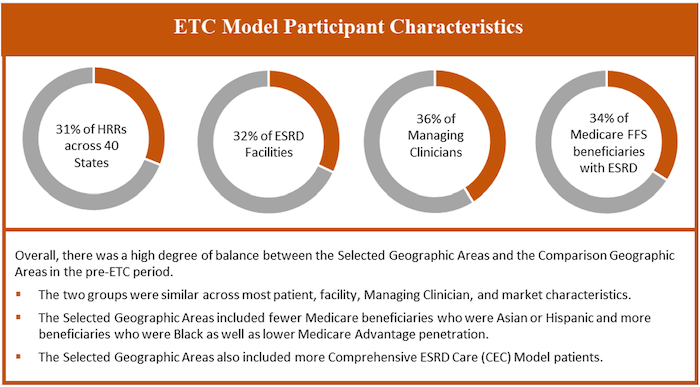
Comparing pre-ETC (2017-2019) and 2021, the ETC model had more Fresenius and fewer DaVita and for-profit independent clinics. Clinics in the South made up 47.3% of those in the ETC Model and 45.2% of non-ETC clinics, while the fewest ETC and non-ETC clinics were in the Northeast. Most (83%) of clinics in both groups were in urban areas. In ETC and non-ETC clinics, there were 5% more Black, 5% fewer non-white Hispanic, 1.5% fewer Asian, and 1.7% more American Indian/Alaska Native patients.
| Clinic Characteristics | ETC Clinics 2017-2019 | Non-ETC 2017-2019 |
|---|---|---|
| Clinics providing PD | 50.6% | 54.2% |
| Clinics providing home HD | 28.8% | 30.4% |
| Total home patients | 7.6% | 8.1% |
The ETC Model led to small changes in home dialysis, in-center self-care and in-center nocturnal dialysis in the first year of the ETC Model.
| Outcomes | ETC Clinics 2017-2019 | ETC Clinics 2021 | Non-ETC 2017-2019 | Non-ETC 2021 |
|---|---|---|---|---|
| Home dialysis | 11.8% | 14.7% | 12.8% | 15.8% |
| • PD | 9.9% | 12.0% | 10.9% | 13.1% |
| • Home HD | 2.2% | 3.0% | 2.2% | 3.0% |
| In-center HD | 88.3% | 85.5% | 87.2% | 84.3% |
| • In-center self-care | .04% | .09% | .02% | .05% |
| • In-center nocturnal | .38% | .25% | .42% | .31% |
| Home dialysis training | .72% | .86% | .76% | .83% |
| Patients say MD & staff gave needed info | 80.2% | 79.9% | 80.5% | 80.2% |
Patient Advisory Group members interviewed in 2022 said dialysis clinics could do more to inform patients about treatment options, to help fearful patients believe they could do home dialysis, and to assure patients about clinic support for home dialysis. They identified that dialysis staff who know little about PD and home HD and staff who made assumptions about candidacy limited growth of home dialysis.
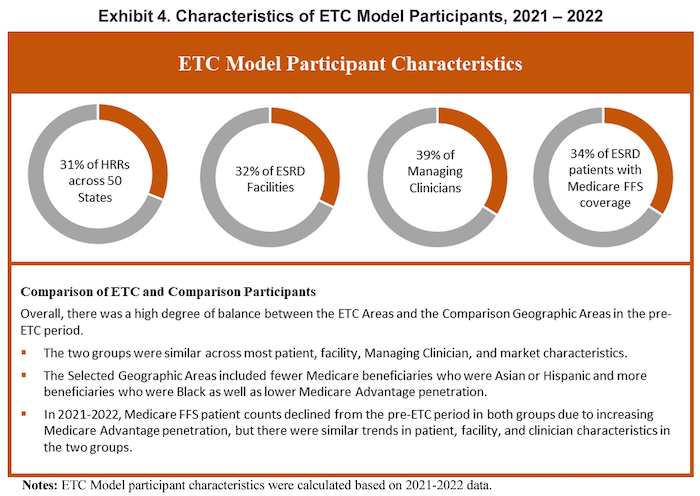
The Second Annual Evaluation Report
In January 2024, the Lewin Group published The End-Stage Renal Disease Treatment Choices (ETC) Model, Second Annual Evaluation Report. There were some changes to the Model in 2022, including efforts to promote health equity and determining how well the ETC Model was serving traditionally underserved populations, i.e., people with Medicare and Medicaid (dual eligible) and those who get the Part D Low Income Subsidy (LIS). The map of HRRs in the Model remained the same. The counts of Original Medicare patients declined, as more patients were in Medicare Advantage plans.
In the pre-ETC period (2017-2019) compared with post-ETC period (2021-2022) for clinics in the ETC Model compared to those not in the Model
| Clinic Characteristics | ETC 2017-2019 |
ETC 2021-2022 |
Non-ETC 2021-2022 | Non-ETC 2021-2022 |
|---|---|---|---|---|
| Clinics providing PD | 50.1% | 49.8% | 54.0% | 53.7% |
| Clinics providing home HD | 28.7% | 28.5% | 30.3% | 30.1% |
| Total home patients | 7.6% | 9.7% | 8.1% | 10.0% |
There was some improvement in the percentages of home dialysis patients and in home dialysis training. Patients in 2021-2022 still said that their MD and staff did not provide enough information for their health needs.
| Outcomes | ETC 2017-2019 |
ETC 2021-2022 |
Non-ETC 2017-2019 | Non-ETC 2021-2022 |
|---|---|---|---|---|
| Home dialysis | 11.8% | 14.9% | 12.8% | 16.0% |
| • PD | 9.8% | 11.9% | 10.8% | 13.0% |
| • Home HD | 2.1% | 3.0% | 2.1% | 3.0% |
| In-center HD | 88.1% | 84.9% | 87.1% | 83.9% |
| • In-center self-care | .03% | .01% | .09% | .04% |
| • In-center nocturnal | .29% | .16% | .33% | .19% |
| Home dialysis training | .70% | .84% | .73% | .81% |
| Patients say MD & staff gave needed info | 80.2% | 79.5% | 80.5% | 79.5% |
The Report provided information about strategies to increase home dialysis and system, provider, and patient-level barriers:
Staffing: Most ETC Model clinics did not hire new staff, but expected existing staff to increase their efforts. Some had regional educators. Many had home dialysis champions. Managing Clinicians described staff shortages as a primary home dialysis barrier.
Patient education: ETC clinics said they increased education about treatment options, including online virtual transitional care program classes. One LDO reported adding home dialysis to its quarterly patient education. Many education efforts were unchanged from prior to the ETC Model. Patient Advisory Group members said education was insufficient.
Capacity: Most ETC clinics with home programs did nothing to increase capacity. Those that did added PD or changed their home HD training room to add PD training. One installed a movable wall to facilitate group home training.
Limited supply storage space: Some ETC clinics and Managing Clinicians did home visits to help patients determine how to fit supplies into limited space. Some sent smaller shipments.
Incentives: Staff were not well informed about the ETC Model or incentives, most of which went to companies, not to individual clinics or clinic staff who want to provide the best possible care for their patients.
Care partners: Frail or elderly patients may need help to move or set up supplies and may need emotional support to cope with home dialysis responsibilities.
Literacy & Language: Educating patients about options and/or training them for home dialysis can require translations and/or verbal or visual demonstrations.
Key Findings of the first 2 years of the ETC Model:
Home dialysis training increased.
Outpatient emergency department use was lower.
Clinical outcomes were no different.
Medicare costs increased for ETC and non-ETC clinics and were only lower for long-term care hospitals and inpatient rehabilitation facilities.
The percentage of PD patients in ETC clinics increased with no significant difference in peritonitis rate.
Vascular access infection rate declined, but was not significantly different in ETC vs. non-ETC clinics.
There was no effect of the ETC Model on mortality.
Home dialysis rates were lower for non-Hispanic Black patients in ETC and non-ETC clinics.
Questions About the Model & Its Effectiveness
The ETC Model has not led to much growth in home dialysis. Home dialysis was already rebounding from many years of stagnation. Reasons why the Model didn’t stimulate more rapid growth could be many and varied.

Was the design of the Model faulty, starting with choosing locations based on Hospital Referral Regions instead of ESRD Networks that have a history of working with dialysis clinics to improve outcomes?
Was it too much to expect dialysis clinics, especially small rural clinics, with no home program to add space to train patients for home dialysis, recruit one or more experienced training nurses, and rent PD cyclers and/or home HD machines with only the hope that enough patients would choose home dialysis to allow the clinic to recoup the added costs?
Would it have been better and resulted in greater growth in home dialysis percentages if CMS had chosen to offer incentives to clinics that had the existing infrastructure, training staff, and equipment when they grew their PD and/or home HD patient population at a higher than average rate?
Would there be better recruitment and retention of home dialysis patients in clinics with larger than average home dialysis patient populations and where training nurses are more experienced compared with clinics that have only a few patients and training nurses have less experience?
Should there have been more incentives to encourage recruitment and hiring of more training nurses to reduce delays in home training that could have allowed interested patients required to do in-center dialysis to become too complacent?
There are many advantages to home dialysis—and there are also challenges. Could ETC Model dialysis clinics do more to identify and address patient-level barriers to home dialysis? What do you think? Feel free to include your thoughts and suggestions in the comments to this blog below.


Comments
James maloney
Aug 20, 2024 4:49 PM
JJTRN
Aug 22, 2024 1:46 PM
As for the prescription itself... no. There really is no cookie cutter standard for how more frequent HD "should be" prescribed. Different practices have different preferences. A good dialysis prescription is a science and an art. In home HD, it's one that can be finely tuned to the individual patients' needs, wants, preferences, and medical goals.
Some companies have prescribing assistance computer programs for their equipment to help figure out what schedules may work best for a person based on weight, labs, and adequacy goals. It's a fantastic starting point, and it can be printed, reviewed, and tweaked. Some patients like every-other-day, we know patients who dialyze every single day too. It is that individualistic, and for great reasons.
I am in favor of any prescription that avoids the usual complications of HD-- including aggressive ultrafiltration and two-day gaps in treatment. :)