A Call to Arms and PD Exit Sites: Please Send Photos to Help Train Home HD and PD Nurses

We have been thinking about home therapies nurse education quite a bit lately at MEI, as we develop online RN education around dialysis (coming soon: stay tuned!). It is clear that a need exists to help nurses new to home dialysis training learn how to take excellent care of home patients. When I was learning, my employer gave me skills modules and tests to complete and I was sent to training seminars, which were great. But, I gained the most knowledge and experience from working 1:1 in bigger programs with experienced home therapies nurses. Not every dialysis nurse has that luxury.
We are Losing Experienced Nurses

Experienced nurses are retiring and taking their repositories of deep knowledge with them, which adds to the chaos patients most certainly notice. Job listings for home therapies nurses include astronomical sign-on bonuses and sometimes even offer to train a new dialysis nurse from the ground up, as staffing continues to be a problem everywhere. Home dialysis is a cool field: nurses who are creative thinkers and enjoy deeply knowing their patients like this type of collaborative work. But, more comprehensive home dialysis information and resources are needed to facilitate expertise.
Many newer home therapies nurses have only been able to assess a small pool of patients they have had access to. It takes variation for clinicians to feel fully confident and capable, which trickles down to patients. This is not the fault of nurses; home dialysis nursing is a microspecialty in a small field, and very little about dialysis is even mentioned in nursing school.
We Need Home Nursing Mentorship
Nurses who find themselves in the home dialysis training space usually crave information and want to improve their knowledge and skills to do better for their patients and help them succeed. I did; that’s why I first found my way to MEI and Home Dialysis Central in the first place. The need for more even more information for nurses in this field is a challenge for staff and patients. Many nurses working in home therapies right now may have never seen some of the most common complications! I think we can fix some of that, and would like to: starting now.
Seeing more patients in more clinics under different circumstances and having an experienced nurse backing me up so I could collaborate and learn even more made a big difference in my practice, and ultimately the trajectory of my life—because now I teach a lot of this and share what I know as much as I can.
I believe the opportunity for similar experiences to mine, with solid peer-to-peer nurse mentorship, is lacking for many of the nurses trying to have successful programs in smaller areas. They don’t get to see as much, can be isolated, are working mostly solo—and in terms of honing nursing assessment and intervention skills, this arrangement just doesn’t advance knowledge as much. The best thing nurses can do to become better at being nurses is to gain experience and to be continually educated.
Seeing is Believing

Home HD nurses may never have seen buttonhole development, fistula skin erosion from hubbing, or excellent one-handed taping and leak prevention firsthand. They may have never seen a solid nocturnal home HD tape job. They may have never needed to locate real estate for sites in a very complicated, twisty fistula and some are working in programs that still prohibit patients with CVCs from going home and may have never seen a CVC exit site maintained by a patient. With the right images, we can address all of this.
I have heard from nurses who are not comfortable teaching rope-ladder cannulation to home HD patients. Some patients have awkwardly placed accesses or mobility or logistical issues and have had to come up with unique workarounds. Newer nurses who haven’t seen this may think these issues are barriers to home care and need exposure to how home therapies as a culture thinks outside the box to find solutions.
Some PD nurses may have never seen a true exit-site infection, inflammation, an extruded cuff, pull/tug trauma, granuloma, tunnel infection, tunnel erosion, tubing tear, adhesive rashes, wet exit sites, skin yeast infections, or wonky catheter positional placement. I am unsure of how many home therapies nurses in smaller PD programs have seen truly healthy or long-term stable exit sites, really good taping techniques for APD, effluent colors—or fibrin, a hernia, a leak, or cloudy versus clear but concentrated bags. These are things that experienced home patients live with every day and are in a unique position to share with professionals who are trying to learn more.
Please Send Photos!
Please ask your patients to share photos if you are a nurse, or please send your photos if you are a patient. Pictures of home HD practices and issues can really make a difference and help us do what we do here at MEI. I wrote a blog about the rainbow colors of PD effluent a few months ago and had to pull images from academic sources, and even those were difficult to locate. We can do better if we get some community help. Can you help us?
We nurses need ways to see if we are learning. We can explain, but it’s much easier when we can show pictures. Photos shared by your patients, with permission, would allow us to start a repository, so we can better teach home dialysis to professionals with real examples. If you have or know patients—please link to and cross-post this blog post as much as you can. I would love to receive as many photos as possible. They will only ever be used for educational purposes and all images will be anonymous. In particular, I am seeking good-quality, clear, and de-identified pictures of:
For Home HD
Accesses that worked, didn’t work, temporary accesses, intervention or progress photos
Cannulation or taping technique for grafts and fistulas at home
EndoAVF arms and needle sites
Any solution that saves time or energy—like making packs or a good organizational system
What you keep in reach, and recommendations if you have any
Unique set-ups or examples of alternative machines or systems
Intradialytic nutrition at home
Blood draw process, so we can teach nurses tricks that work better
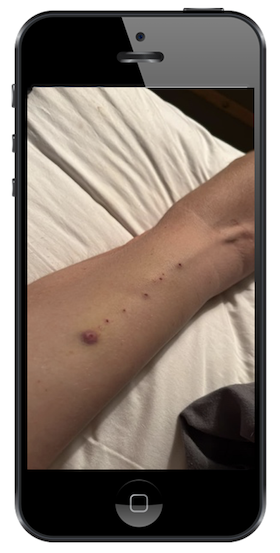
Examples of infections, skin/tape irritation or breakdown
Clotted systems, mishaps, tricks to keep a line open
For PD
PD exit sites in all conditions, and stages of healing, including perfect and near-perfect. Explanations are welcome if there is something going on in the picture we can point out
Sensible-tape and immobilization solutions for PD catheters—especially ones others might want to replicate. Belts? Tabs? Share pictures of what works
Dressings—post op, healing, securing a PD catheter without dressings
Skin or tunnel complications of any kind.
Surgical photos or X-rays of catheter placement or repositioning
PD fibrin in any forms
PD effluent that is clear, cloudy, concentrated, or colored.
Blood in a PD bag (hemoperitoneum) from women with menstrual cycles
Storage or organizational solutions you’re pleased with
I would like to help better equip nurses to help home patients by giving them education that has photos of real people to help them learn assessment. Even if you’re reading this 5 years from now—please, jump in! Send photos—and a quick permission statement (e.g., “I give the non-profit MEI permission to use this photo for educational purposes.”)—to Photos@mei.org.


Comments