Ultrafiltration Rates in Hemodialysis and a Reply to John Agar

Standard In-center Hemodialysis Unphysiology
Many of us who work in nephrology know that removing water too quickly during hemodialysis does serious, systemic damage—and there is a strong link between high UF rates and death. This connection is a frequent topic in home dialysis circles. One of the most profound elephants in the in-center HD room is the disconnect between understanding that fluid balance is vital for survival, yet trying to restore fluid balance at rapid, unphysiologic rates.
One reason we focus so much on home dialysis at MEI is because U.S. dialysis is designed to provide treatment en masse, as a lot of people need treatment. But, standard HD is not routinely physiologically tailored to individuals, particularly when done just three times/week. (There are historic reasons for the U.S. in-center HD treatment schedules that go back 50 years—see Less Hemodialysis is NOT More). Patients who learn how dialysis works to remove water and wastes may be more likely to choose longer, slower, more frequent, more physiologic treatment. With gentler treatment, patients can feel better, be more productive, and perhaps live longer. Well-trained home HD patients view the time trade-off as worth it, and we keep sharing this. I wrote my own spin on the subject in, The Truth About Home Dialysis Time. There are so many posts about the benefits of more HD that we hope this is not “secret” knowledge any more!
Dr. Agar—the Man, Myth, and Legend

This Halloween, we re-ran a blog post by Dr. John Agar from June of 2016: Haemodialysis UF Volume and UF Rate are NOT the Same. To briefly re-cap:
UF volume is the total amount of water that is “goaled for” during a single treatment to return a person to estimated dry weight.
UF rate is the speed by which the volume of water is removed.
I really don’t need to explain this further. The post is a great read. We were pleasantly surprised to see last week that the man, myth, and legend himself—John Agar—replied to his blog: a super rare occurrence these days. John is elusive and now retired to the point where he’s more likely to write novels than consult on kidneys. Here is what he said:
“It is strange to find myself agreeing with myself after all these years…that perhaps I didn't go far enough as I would probably now fancy <8 ml/kg/hr [rather than <10] as a safe rate, but then I have retired and been out of the game for nearly 5 years and have not really been keeping up with the literature. Others may have subsequently refined this target with greater precision.
Still, I must thank Dori for running this rather naive post again – as it does make some useful points. I really wish I knew [1] if people read these posts and 2] whether dialysis services have [broadly] taken on this message and are now extending their hours and slowing the ultrafiltration rate they use. But, my natural pessimism nags at me and whispers that they are probably not. If so, this would be to the detriment of patients everywhere.”
I was so overjoyed to see his name pop up that I momentarily forgot how sad the lack of progress on this issue makes me. I started to reply in comments several times, then quickly realized I was about to hop on my soapbox and leave him a long-winded and sentimental comment that would be better off delivered as its own blog post! Usually, when I go off on a tangent, Dori inevitably tells me to blog about it anyway, so I can hear her in my head. I was going to reply with something like…
Dear John,
We still agree with you too. You’re right, and the education you’ve done on this continues to save lives—especially in the US, where I am sad to report very little has changed on a broad scale outside of home dialysis, which still has not become the industry norm.
These blog posts come up in Google searches and folks continue to find them. Hopefully people still appreciate human writing vs. AI. We like to think that keeping these posts here still influences change and saves lives. That’s still important to us at MEI, even if it has not yet changed the entire industry. We do always start with hope…right?
We would also much prefer to see <8mL/kg/hr be the maximum UF rate rather than <10mL/kg/hr. Long live the mantra, “Low and slow is the way to go.”
I’m not sure if you heard that last year, CMS elected to remove the >13mL/kg/hr UFR reporting measure from the ESRD Quality Improvement Program (QIP). Beth Witten wrote about that (and other new changes) in A Quick Summary Of 2024 Medicare Changes That Affect Dialysis Patients. They are tracking time-on-machine now, but not (to my knowledge) in relation to UF volume. I am also not sure how the loss of that reporting measure will affect practice. It concerns me, as 13mL/kg/hr was already too outrageously high. I don’t know where the number 13 came from in the first place…perhaps it was selected for being unlucky? That would almost make sense.
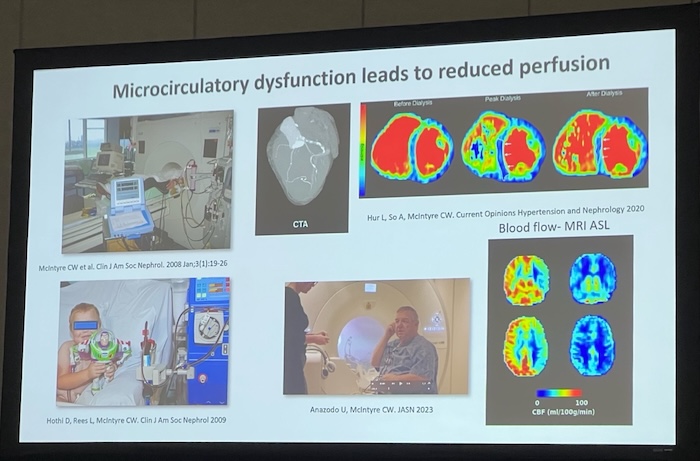
Dori recently posted ASN Kidney Week 2024 Through A Home Dialysis Lens. Dr. Chris McIntyre gave an awesome talk about organ stunning. He had fantastic slides and included videos of what happens to muscle during dialysis from whole body scans taken during treatment. I had not seen that before outside of my own conceptual vision, and it was quite profound. I’d say it was cool, but it’s pretty sobering to see.
Obviously, we knew some of what we would hear. The link between excessive UF and ischemic organ and tissue damage needs to be shouted from the rooftops.
Apparently, you are feisty and righteous, and that type of energy is so needed again. We’re in a whole new era of the fight, and could use louder voices about these basic fundamentals. Organ stunning is still relevant and requires oversight.
In truth, we continue to share new blogs just about weekly and often refer back to classic posts like yours. We are always happy to tell patients the things they need to know to not just survive but thrive on dialysis. For the most part, there is room for improvement in U.S. standard in-center HD and there are, as there always have been, exceptions. The exceptions are our true allies.
Thank you for the countless hours you have spent educating about this.
Always trying,
Jennifer
To those reading, thank you. If you are reading this blog for the first time, or are looking for suggestions on which blogs to read next, there’s a great list here: Lessons From Across The Top 9 KidneyViews Blog Posts


Comments
John Agar
Sep 23, 2025 10:41 PM
John
Prof John W Agar
Sep 21, 2025 1:00 PM
Thank you so much
John
John Agar
Apr 09, 2025 12:30 PM
I have just happened upon your very generous post. My thanks for supporting my argument[s]. I saddens me that so few understand the simple physiology that says 'if you remove fluid from the circulatory volume faster than the extra-circulatory tissues can replace it, the circulation is in danger of [and will] collapse'. Its physiology 101. PS: retirement is wonderful .... and - as a blatant promotional hint - you can buy my book 'Second Sons' on Amazon and Kindle with a sequel in preparation!
Olive Gorringe
Dec 12, 2024 12:05 AM