Home Dialysis Updates from the 2024 USRDS Annual Data Report

Each year, the National
Institute of Diabetes and Digestive and Kidney Disease (NIDDK) funds
publication of an annual data report (ADR) on kidney disease.1 Data are collected from CMS, the
United Network for Organ Sharing (UNOS), and the ESRD Quality Reporting
System (EQRS). The ADR has chapters on chronic kidney disease (CKD) and
on end stage renal disease. As it takes time to collect and analyze
data, the most recent ADR has data from 2 years ago. Since 2021,
the ADR has included a chapter on home dialysis.
 We have
published two prior blogs about these data. The first
blog (2009-2019 data) was published in March, 2022 and the second
blog (2010-2020 data) in January, 2023. This blog will provide some
data changes over time and some new data you may find
interesting.
We have
published two prior blogs about these data. The first
blog (2009-2019 data) was published in March, 2022 and the second
blog (2010-2020 data) in January, 2023. This blog will provide some
data changes over time and some new data you may find
interesting.
Viewing the Data
The 2024 ADR Chapter 2 has multiple ways to learn about adults on home dialysis. There is a bullet list of new things the researchers looked at as well as data highlights. The introduction describes where the data come from and how home patients are identified. Figures of interactive graphs allow you dive deeper into the data. Finally, you can see reference tables that support the text and figures. Below is a list of figures in the 2024 ADR; blue type indicates new data:
Figure 2.1a - Utilization of home dialysis in adult dialysis patients, overall and by modality, stratified by ESRD status, 2012-2022
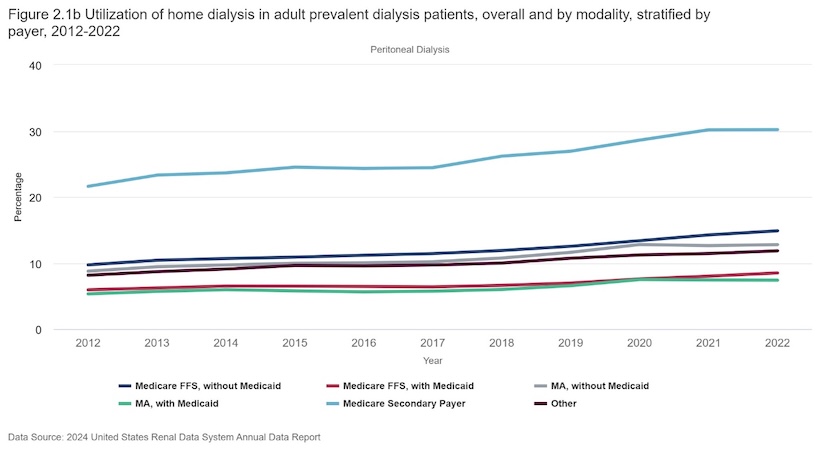
Figure 2.1b - Home dialysis utilization, by payer, 2012-2022
Figure 2.2 - Home dialysis utilization by ETC
Figure 2.3a - PD utilization by HSA, 2022
Figure 2.3b - HHD utilization by state, 2022
Figure 2.4 - Access to home dialysis, 2017-2022
Figure 2.5 - Home dialysis patients per certified facility, 2022
Figure 2.6 - Patient characteristics, 2022
Figure 2.7 - PD patient characteristics, 2012-2022
Figure 2.8 - Physician specialty of PD catheter insertion, 2012-2022
Figure 2.9 - Duration of ESRD at home dialysis initiation, 2018 and 2022
Figure 2.10 - PD initiation within 7 days of catheter placement, 2012-2022
Figure 2.11a - HHD treatments per week, 2022
Figure 2.11b - HHD session duration, 2022
Figure 2.11c - HHD hours per week, 2022
Figure 2.12 - Complications on PD, 2012-2022
Figure 2.13 - Complications on HHD, 2012-2022
Figure 2.14 - Conversion from home dialysis to ICHD, 2012-2021
Figure 2.15a - Receipt of HD within 30 days after admission to SNF, 2012-2022
Figure 2.15b - First dialysis modality after discharge from SNF to home, 2017-2022
Figure 2.16 - Mortality after home dialysis initiation, 2020-2021
Figure 2.17 - Waitlist prevalence, 2022
Figure 2.18 - Kidney transplantation after home dialysis initiation, 2020-2021
Figure 2.19 - Outcomes after home dialysis initiation
Changes to the Percentage of Patients on Home Dialysis Over Time
In the 2024 ADR, Figure 2.1a shows changes in home dialysis modalities and demographics each year from 2012-2022, with one graph for incident and one for prevalent patients. Each graph allows you to choose “home dialysis,” “PD,” or “Home HD.” You can drill down to see data for each modality overall, by age (4 options), sex (2 options), race/ethnicity (5 options), primary cause of ESRD (5 options), social deprivation index (3 levels), or rural/urban status. Or, if you prefer, you can read the text describing those data.
From 2012-2022, the percentage of incident patients starting home dialysis overall (PD and home HD) increased by 70% from 8.5% to 14.5%:
Incident patients on PD increased by 69%, from 8.3% to 14.0%.
Incident patients on home HD increased by 33%—from 0.3% to 0.4%.
Among prevalent patients, the percentage of home dialysis overall grew by 42%, from 10.2% to 14.5%:
Prevalent patients on PD increased by 37.5%, from 8.8% to 12.1%.
Prevalent patients on home HD increased by 60%, from 1.5% to 2.4%.
Patients More (or Less) Likely to use Home Dialysis
Have you ever wondered how likely it is for a patient with high social needs to access home dialysis? This ADR includes a social deprivation index (SDI) from responses to the American Community Survey. SDI is based on elements such as living in poverty, no high school diploma, in single parent households, renters, overcrowded housing, lack of a car, and under 65 and unemployed. Those with higher SDI check more of those boxes. Figure 2.1a discusses other demographics as well as SDI and home dialysis utilization:
Age: Incident and prevalent PD and home HD patients were more likely to be younger.
Sex: A similar percentage of males and females were on PD in both incident and prevalent patients. Incident home HD patients were similar. Among prevalent home HD patients, there were slightly more males.
Race: Among incident and prevalent PD patients, the order by percentage was Asian, White, Other, Hispanic, then Black. Among incident home HD patients, the order was Other, White, Asian, Black, Hispanic. Among prevalent home HD patients, the order was White, then Black, Other, Asian, then Hispanic.
Primary cause of ESRD: Interestingly, among incident and prevalent PD patients, the most common cause was cystic kidney disease. People with diabetes were less likely to use PD or home HD.
Social deprivation index: Those with the highest SDI were less likely to start or be on PD as incident or prevalent patients. A small, similar percentage of incident patients in each SDI group started on home HD. Among prevalent patients, those with the highest SDI were about half as likely to be on home HD as those with the lowest SDI.
Rural vs. urban: Rural patients were slightly more likely to start and be on PD or home HD.
Payment Source and Home Dialysis
I’ve always been interested in how the source of payment might affect who does home dialysis. Figure 2.1b (below) shows this graphically. As you can see, a higher percentage of patients insured by job-based plans with Medicare as a second payer did home dialysis. The next most likely group had Original (Fee for Service) Medicare without Medicaid. Finally, those who had Medicare Advantage without Medicaid were less likely to use PD or home HD. Those least likely to do home dialysis had Medicaid as a second payer. Patients with Medicaid are (not surprisingly) more likely to have high SDI.
Availability of Home Dialysis
A new data element in the 2024 USRDS relates to infrastructure and human capital (Figure 2.4). From 2017 to 2022, the number of dialysis clinics increased by almost 10%. Yet, as you can see in the table below, despite the Executive Order and CMS efforts to encourage home dialysis, 57.9% of U.S. dialysis clinics were not certified to offer home dialysis training and support, or were certified—but had no home patients in 2022. This may help explain so many patients only have the choice of standard in-center HD when PD is no longer adequate.
| Home Clinic Status | 2017 | 2022 |
|---|---|---|
| Certified for home & actively treating home patients | 42.3% overall 40.5% PD; 16.5% Home HD |
42.1 overall 40.1% PD; 17.3% Home HD |
| Certified for home, but no home patients | 12.1% overall 12.5% PD; 13.4% Home HD |
11.3% overall 11.5% PD; 11.9% Home HD |
| Not certified for home | 45.7% overall 47.0% PD; 48.6% Home HD |
46.6% overall 48.6% PD; 70.8% Home HD |
Typical Numbers of Home Patients Treated Per Clinic
Figure 2.5 examines the number of patients treated by clinics that are certified to train and support PD and/or home HD. More than 22% have no PD patients and more than 40% have no home HD patients. Most dialysis clinics certified to train and support home patients have 10 or fewer patients. Only about 10% of clinics have 31 or more PD patients, and fewer than 6% of clinics have 21 or more home HD patients. Per the USRDS, dialysis facility program size may affect outcomes. This seems logical, since programs with more patients are likely to have physicians and staff who are experienced and supportive of home patients. Indeed, one study found that smaller PD programs have higher PD discontinuation rates.2
| Figure 2.5 Number of Home Dialysis Patients Per Certified Facility, by Modality, 2022 | |||
|---|---|---|---|
| Number of patients | Home Dialysis | Peritoneal Dialysis | Home Hemodialysis |
| 0 | 21.23 | 22.24 | 40.76 |
| 1-10 | 26.79 | 30.85 | 43.91 |
| 11-20 | 22.31 | 22.50 | 9.79 |
| 21-30 | 12.20 | 11.22 | 2.94 |
| 31-40 | 6.50 | 5.82 | 1.05 |
| 41-50 | 4.00 | 2.69 | 0.55 |
| 51+ | 6.96 | 4.68 | 1.01 |
Patients Who Switched from PD or Home HD to In-center HD by 24 Months
Figure 2.14 provides data on switches to ICHD related to home program size. PD programs were divided into those with <11 patients, 11-20 patients, and >20 patients. In 2022, 36.6% of PD patients had switched to ICHD programs by 24 months in programs with <11 patients, a 20% higher dropout rate than in programs with >20 patients (30.5% had switched).
That same year, home HD programs were divided into those with <6 patients, 6-10 patients, and >10 patients. In 2022, 43.9% of patients in clinics with <6 home HD patients had switched to ICHD by 24 months, a 19% higher dropout rate vs. 37% who had switched in home HD programs with >10 patients.
The ESRD Treatment Choices Model set out to promote home dialysis. However, over the past 4 years it has failed to yield the desired results. In fact, this model may have unwittingly contributed to under-resourced clinics attempting to start home programs that did not grow large or fast enough for staff to gain the requisite experience to adequately train and sufficiently support home dialysis patients. This dynamic may have contributed to patient dropout and return to ICHD, which is costly and demoralizing to patients and staff.
Conclusion
This blog reported on only a fraction of the data you can find in the USRDS Annual Data Report. I urge you to take a look. You may find something that piques your interest and leads you to write a blog or take a stab at doing a research project with your patients. The sky’s the limit!
United States Renal Data System. 2024 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2024. https://usrds-adr.niddk.nih.gov/2024/end-stage-renal-disease/2-home-dialysis↩︎
Young, E. W., Kapke, A., Ding, Z., Baker, R., Pearson, J., Cogan, C., Mukhopadhyay, P., & Turenne, M. N. (2019). Peritoneal Dialysis Patient Outcomes under the Medicare Expanded Dialysis Prospective Payment System. Clinical journal of the American Society of Nephrology : CJASN, 14(10), 1466–1474.↩︎


Comments